Fra PathologyOutlines.com Lymes disorders
https://www.pathologyoutlines.com/topic/skinnontumorlymedisease.html
The Myths of Lyme Disease: Separating Fact from Fiction for Military Personnel > National Defense University Press > News Article View https://ndupress.ndu.edu/
Fakta og hypoteser om nye trusler fra naturen
Spirocheter, Borrelia og udiagnostisert kronisk borreliose (Hentet fra Biolog-2013- Laane-MM.pdf
https://epidemi.no/wp-content/uploads/2013/11/Biolog-2013-Laane-MM.pdf
Hentet fra Bioingeniøren
Forsker Brorson
Øystein Brorson er garantert den bioingeniøren i Norge som vet mest om bakterien Borrelia burgdorferi. Han er kanskje DEN som vet mest. Daglig får han henvendelser fra hele verden om forskningen sin. Interessen fra fagmiljøene i Norge er ikke like stor.
PUBLISERT
ENDRET

Øystein Brorson var den første i verden som fant ut at cysteformen av Borrelia burgdorferi kan omformes tilbake til vanlige, mobile mikrober. Dette er ifølge Brorson et viktig funn fordi det betyr at behandlingen av borreliose må revurderes. De tradisjonelle antibiotikatypene tar nemlig ikke cystene.
– Siden har flere påvist det samme. En italiensk forsker som podet cyster på mus, fant at musene fikk borreliainfeksjon. Annen forskning har vist at cysteformene av bakteriene kan opptre tidlig i sykdomsforløpet. Det betyr at leger bør vurdere en såkalt kombinasjonsbehandling også for pasienter med tidlig borreliose, mener han.
Ting tar tid
Men det er som kjent ikke lett å bli profet i eget land. Selv om forskeren Willy Burgdorfer, han som fant bakterien første gang på begynnelsen av 80-tallet, har henvist til Brorsons arbeid og rost det, er de norske fagmiljøene heller lunkne. Brorsons resultater har ikke ført til endringer i behandlingen av borreliosepasienter.
– Ting tar tid, spesielt innen medisin. Medisinere er nemlig konservative. De skal være skeptiske, men burde nok samtidig være litt mer åpne for ny viten. På min egen arbeidsplass samarbeider jeg godt med seksjonsoverlegen ved Infeksjonsmedisinsk avdeling, Per Bjark. Han kan svært mye om borreliose og regnes som Norges fremste kliniker på området. Vi er enige om at behandlingen bør legges om. Her i Tønsberg blir pasienter som ikke blir bra av konvensjonell behandling henvist til infeksjonsmedisinsk avdeling. Der får de som oftest kombinasjonsbehandling. Jeg tror vi er de eneste i landet som gir det. I USA derimot, er det blitt svært utbredt, forteller Brorson. Han er påpasselig med å nevne en annen Brorson. Fetter Sverre-Henning, som er bioingeniør, cand scient, PhD og spesialist i elektronmikroskopi, har vært en svært viktig samarbeidspartner i forskningen, forteller han.
Sirkulerende immunkomplekser
Brorsons interesse for borreliose ble vakt da han leste Willy Burgdorfers originalartikkel fra 1982 om bakterien som senere fikk forskerens navn.
– Siden jeg jobber og bor midt i flåttbeltet var dette spennende lesing. Vi var raske til å innføre testene etter hvert som de kom. Og det var spesielt viktig å kunne ta i bruk testen som påviser spesifikke sirkulerende Borrelia burgdorferi immunkomplekser, sier Brorson.
Han forteller at det ikke er uvanlig å få negative antistofftester selv om det er sterk mistanke om borreliose. Årsaken er at alle antistoffene kan være bundet opp i immunkomplekser. Brorson og kollegene tok derfor allerede 1990 i bruk en metode som løser antistoff og antigen fra hverandre og som derfor gjør det mulig å måle det bundne antistoffet. Metoden fungerer samtidig som en indirekte antigentest.
– Vi har funnet ganske mange pasienter som er positive på denne testen selv om de tester negativt på vanlig antistofftest, forteller han.
Han har ikke noen god forklaring på hvorfor Mikrobiologisk avdeling i Vestfold fremdeles er den eneste i landet som utfører denne testen, men han forteller at det fra tid til annen kommer prøver fra universitetssykehusene.
MS-forskning
I 2002 fikk Brorson en forskningspris fra Helse Sør. Den var på 200 000 kroner og i begrunnelsen sto det blant annet at ”Brorson har på en forbilledlig måte grepet fatt i et helseproblem som er spesielt for vår region og søkt å belyse dette med nytenkende forskning”.
En av grunnene til at han fikk prisen var sannsynligvis forskningen på sammenhengen mellom multippel sklerose (MS) og Borrelia burgdorferi. Høsten før han fikk prisen, publiserte han nemlig en artikkel som vakte oppsikt. I den beskrev han en undersøkelse av ti pasienter med MS. Det viste seg at alle ti hadde cysteformer i spinalvæsken. Han klarte ikke å bevise med hundre prosent sikkerhet at det var Borrelia burgdorferi cyster, men han sannsynliggjorde det.
– Åtte av de ti pasientene var med i videre undersøkelser. Vi ga dem ulike kombinasjonsbehandlinger og det viste seg at den ene typen resulterte i at cystene ble borte. Under behandlingen ble et par av pasientene mye bedre, men bedringen gikk delvis tilbake etter at behandlingen var avsluttet, forteller han.
Selv om ikke resultatene var helt overbevisende, har Brorson lyst til å fortsette undersøkelsene på MS-pasienter. Han har fremdeles stor tro på at Borrelia burgdorferi kan være den egentlige årsaken til en del MS-diagnoser.
– De pasientene som var med i undersøkelsen hadde hatt MS i mange år og vi vet ikke om det hadde oppstått irreversible endringer i nervesystemet. Jeg ønsker meg derfor en ny undersøkelse med pasienter som nylig har fått MS-diagnosen.
Ingen planer om doktorgrad
Øystein Brorson er 1. lektor ved Høgskolen i Østfold. I tillegg er han overbioingeniør ved Avdelig for mikrobiologi i Tønsberg. Til begge de halve stillingene ligger det en del forskning, og per i dag utgjør forskningen 40 prosent av arbeidstiden hans. Til høsten kan det bli mer.
– Høgskolen i Østfold har bestemt seg for at mikrobiologi- og patologiundervisningen bare skal gis i Østfold fra høsten av. Det betyr at jeg ikke skal undervise studentene lenger her i Vestfold. Den halve stillingen ved Høgskolen kommer derfor forhåpentligvis i sin helhet til å knyttes til FoU-arbeid, forteller han.
Det kommer derfor etter all sannsynlighet til å komme flere forskningsresultater og publiseringer om Borrelia burgdorferi fra Brorson i framtiden. Men noen doktorgrad har han ingen planer om, selv om han har publisert mer enn nok artikler om emnet til å disputere.
– Grunnen til at jeg skriver artikler for internasjonale tidsskrifter er at jeg ønsker at alt som oppdages om dette emnet skal nå bredt ut. Det er nemlig viktig for at pasientene skal få så god behandling som mulig. Om det resulterer i en doktorgrad for meg er mindre viktig.
Stikkord:
https://www.youtube.com/watch?v=TLP_q2JSSAY
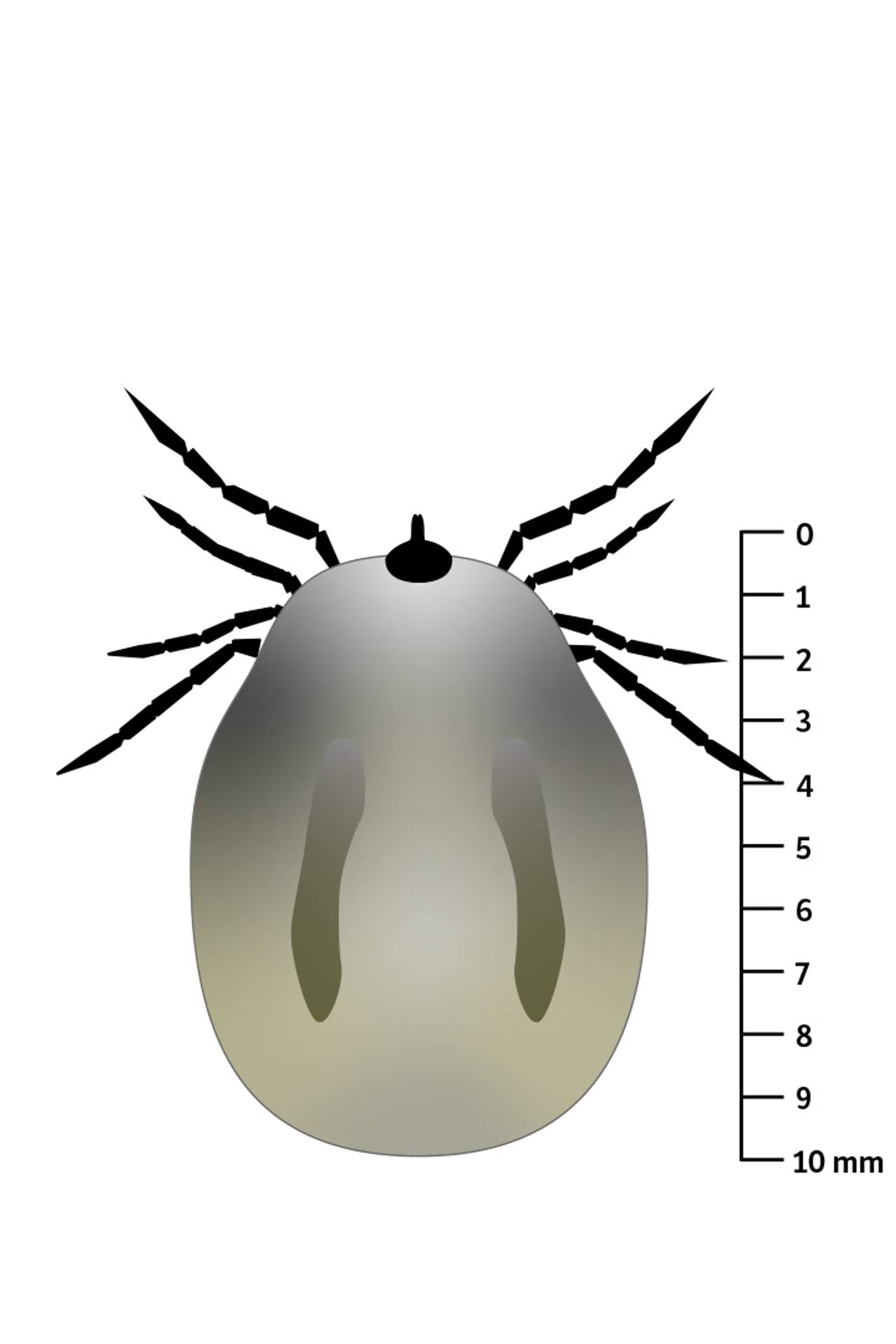
Jaktflått oppdaget for første gang på pattedyr i Norge. Nettavisen

Den er tre ganger så stor som vanlig flått og kan gi alvorlig sykdom hos mennesker.
Arten er nå funnet på et pattedyr i Norge. Ekspertene ber folk være observante hvis de finner flått som ikke ligner på norske flåttarter.
– Jaktflåtten Hyalomma marginatum ble i høst påvist på en hest i Vestby kommune. Dette er en jaktflått, en art som oppsøker vertsdyr, sier biolog Yvonne Kerlefsen ved Flåttsenteret til NTB.
– Kan gi alvorlig sykdom
Mens vanlig norsk skogflått sitter stille i busker og på gress og biter seg fast i forbipasserende vertsdyr, er jaktflåtten tre ganger så stor og løper etter byttet sitt. Som om ikke det var nok, kan kjempeflåtten bære med seg hemoragisk krimfeber – Crimean-Congo Haemorrhagic Fever (se faktaramme).
– Viruset kan gi alvorlig sykdom hos mennesker og har en dødelighet på rundt 30 prosent. Sykdommen er utbredt i Midtøsten, Afrika og Asia. Man har sett noen tilfeller i Sør-Europa, men dette er heldigvis ikke en sykdom vi har i Norge, sier Kerlefsen.
Hemoragisk feber betegner flere ulike virusinfeksjoner, blant annet ebola. Sykdommene er vanligvis ikke beslektede. De gir karakteristiske symptomer med kraftige blødninger og høy dødelighet, og har forekommet spesielt i tropiske og subtropiske land.
Les også: Flåttsmitte: Får du dette utslettet, er det én behandling som gjelder

Tre ganger større
Personen som sendte inn flåtten, skal ha stusset over utseendet.
Denne flåttarten er lett å skille fra vår vanlige skogflått på grunn av størrelse, farge, samt at den har hvite ringer på beina. Rapporter fra Europa tyder på at jaktflått er i ferd med å spre seg nordover. Den er vanligst i Asia og Midtøsten, men har også etablert seg i deler av Sørøst-Europa. De siste årene er den funnet sporadisk i Nord-Europa.
– Jeg var 90 prosent sikker da jeg så bildet av flåtten, men for å være sikker ble den sendt til en veterinær som identifiserte den under mikroskop, sier Kerlefsen.
Ingen vet hvordan hesten i Vestby kommune har fått på seg flåtten. Flåttarten transporteres hovedsakelig til nye områder med pattedyr eller trekkfugler, og har til nå kun vært observert sporadisk på trekkfugl. I likhet med insekter og edderkopper kan flått også importeres i last og bagasje.
– Hesten har ikke vært utenlands, sier Kerlefsen.
Les også: Flåttsmitte: Får du dette utslettet, er det én behandling som gjelder
Ber folk ta bilde
Hvis man oppdager uvanlige flått, oppfordres folk til å ta bilde av flåtten, ta vare på den hvis mulig, og kontakte Flåttsenteret.
– Vi tror ikke den er i ferd med å etablere seg i Norge, men det kan være noe underrapportering, sier Kerlefsen.
Klimaendringer som i særlig grad medfører varme somre, kan føre til at nye flåttarter, inkludert jaktflåtten, på sikt vil kunne etablere seg.
Rapport og innsendelse av uvanlige flåttarter kan bidra til bedre oversikt og kan gjøres til Flåttsenteret, Folkehelsa eller NMBU Veterinærhøgskolen.
https://www.nrk.no/viten/vaksine-mot-flatt-og-alle-flattbarne-sykdommer-1.15587425
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7390863/
NCBI. PMC. US National Library of Medicine National Institutes of Health
A Practical Approach to the Diagnosis of Lyme Borreliosis: From Clinical Heterogeneity to Laboratory Methods
Abstract
Clinical evaluation of Lyme Borreliosis (LB) is the starting point for its diagnosis. The patient’s medical history and clinical symptoms are fundamental for disease recognition. The heterogeneity in clinical manifestations of LB can be related to different causes, including the different strains of Borrelia, possible co-infection with other tick transmitted pathogens, and its interactions with the human host. This review aims at describing the heterogeneous symptoms of Lyme Borreliosis, as well as offering a practical approach for recognition of the disease, both in terms of clinical features and diagnostic/research tools.
Introduction
The genus Borrelia includes three Groups: Lyme Borreliosis (LB), Reptil Associated (REP), and Relapsing Fever (RF) Group (1).
Lyme disease or Lyme borreliosis (LB) is an anthropozoonosis, caused by different genospecies of the Borrelia burgdorferi sensu lato complex. The main tick vector for Borrelia species in Europe is the Ixodes ricinus (2), in America the Ixodes scapularis and Ixodes pacificus (3–5), while in Asia (6) and Russia (7) it is the Ixodes persulcatus. These ticks are possible vectors of Lyme Borreliosis (LB) as well as other pathogens, including viruses, intracellular bacteria, and Protozoa which can co-infect humans (LB co-infections) (8, 9). There are several B. burgdorferi sensu lato genospecies, directly associated with human LB. However, only three genospecies, namely Borrelia burgdorferi sensu stricto, B. afzelii, and B. garinii, have been systemically related to LB (4, 10). In addition, four other genospecies have been occasionally detected in humans: B. bissettiae (4, 5), B. lusitaniae (6, 7), B. spielmanii (8), and B. valaisiana (9), especially in Europe (11). Specificity in terms of dominating hosts has been reported both across and within continents (12, 13). The spatial distribution of the different genospecies allocates Borrelia burgdorferi sensu stricto in North America [and possibly B. mayonii, although this causes a disease somewhat distinct from typical LB (14)] and five species in Europe and Asia, B. afzelii, B. garinii, B. burgdorferi, B. spielmanii, and B. bavariensis (15). The heterogeneity in terms of genospecies can mirror different clinical manifestations of LB due to host specialization and tissue tropism. Although overlapping, distinct spectra of clinical manifestations have been recognized for the three main genospecies. In detail, B. burgdorferi sensu stricto is mostly associated with arthritis and neuroborreliosis, B. garinii with neuroborreliosis, and B. afzelii with chronic skin conditions such as acrodermatitis chronica atrophicans (10).
Spirochetes circulate in small amounts in the blood even in acute LB patients (16), with the exception of Borrelia mayonii which has been reported to cause high spirochetemia (14, 17). Depending on the case and genospecies, they can grow in several tissues (18), including skin, nervous and joint system, although less frequently LB can also affect eyes, heart, spleen, and other tissues.
Based on the spatial variability of Borrelia, for an accurate diagnosis, it could be useful to know if the patient has visited other countries or continents.
Some clinical aspects that can be helpful for a correct diagnosis of LB will be described hereafter. Figure 1, instead, shows an overview of possible overlapping scenarios defining LB. Furthermore, a brief description of laboratory investigation tools is included at the end of the review.
Tick-Bite Without Erythema Migrans
Patients sometimes seek medical assistance after a tick bite. In this case, the first step is to remove the tick with small tweezers or an ad hoc tool at the level of the rostrum. Afterwards, it is important to inform the patient of the symptoms, which, in the case of Borrelia infection, may develop in days/weeks. It is also possible to submit the tick for identification and testing for different pathogens. The identification of pathogens within the tick defines a possibility, not the certainty of developing LB (19).
Erythema Migrans (EM)
Recognition of an EM rash is very important in LB as it is a hallmark symptom of LB, even when the patient does not recall the tick bite. However, as it has been observed, in rare cases the tick can still be attached to the center of the EM (20, 21). The geographical area where the patient was bitten as well as the date are important elements that should be gathered from the patient. Other variables to establish are: the time elapsed between the tick bite and the appearance of the erythema (usually 5–30 days) and its diameter, especially if larger than 5 cm (22). The most important diagnostic criterion is the EM centrifugal evolution. Erythema migrans (Figure 2) is pathognomonic for LB, therefore it should be treated immediately as serology testing to confirm infection is not necessary. Nevertheless, the clinical presentation of an EM can vary considerably (23). Several clinical variations have been observed, such as smaller-sized-EM of about the size of a coin, oval shaped EM with no darker outline, red-violet EM (erysipeloid), EM with vesicles which mimics herpes simplex or herpes zoster (24), painful EM (burning), itchy EM, hidden EM (scalp), and EM with atrophic evolution (25). It has been shown that in some cases of EM, Borrelia infection can already be disseminated (26).

Erythema Migrans of the thigh.
Differential diagnoses include: mycosis fungoides, granuloma annulare, and interstitial granulomatous dermatitis (IGD), tinea corporis (mini EM), and erythema necroticans migrans.
Serological testing is not recommended because of their poor sensitivity in the early stages of LB. In order to achieve the best outcome for patients, antibiotic treatment should be started without delay.
Cutaneous Manifestations Excluding the Erythema Migrans
Multiple Annular Erythema
Secondary EM is characterized by multiple erythematous lesions, which do not develop round the site of the tick bite. It can consist of a few or several plaques that can be located throughout the body (27). The lesions are multiple and can vary from a few cm to more than 20 cm, and are more frequently observed in children (22). The presence of multiple annular erythemas may precede the onset of neurological manifestations, especially in adults.
Borrelia Lymphocytoma
Borrelia lymphocytoma is defined as a B-cell pseudo-lymphoma that occurs in response to the presence of Borrelia antigens in the skin. Borrelial lymphocytoma can develop when EM is present and mimics a tick-bite reactive nodule. It is relatively frequent in Europe, while it is seldom observed in the US, because in most cases it is caused by Borrelia afzelii and more rarely by B. garinii and B. bissettii (28). Clinically, it appears as a solitary (rarely multiple) soft and non-tender bluish-red nodule or plaque with a size between 1 and 5 cm, sharply demarcated. It is typically found on the ear lobe (Figure 3), the mammary areola, and less frequently on the scrotum or the axillary fold. Extra-cutaneous signs and symptoms are very infrequent. The presence of Borrelia biofilm in human infected skin tissues has been demonstrated (29).

Borrelia Lymphocytoma of the ear lobe.
In the presence of this clinical manifestation the following exams should be performed: serology for Borrelia burgdorferi (ELISA and Western-Blot), β2-Microglobulin, and serological tests for Ehrlichia (Anaplasma) (30). Histological examination of skin biopsy and immunohistochemistry to define immunophenotype are also suggested (usually CD20 positive, Bcl-2 negative, κ and λ light chain expressed in an equivalent manner and Borrelia-PCR on DNA from skin slides).
Differential diagnosis includes cutaneous marginal zone lymphoma (PCMZL, Figure 4), which clinically and histologically may present similarities at the immunophenotype. PCMZL is generally CD20, CD22, CD79a, and BCL-2 positive, whereas it is CD5, CD10, Bcl-6, and CD23 negative, and the κ/λ light chain ratio in the histological tissue is very high (31). Borrelia’s detection in PCMZL is included in the EORTC guidelines (32, 33).

Primary cutaneous B cell marginal zone lymphoma of the trunk. Of note the image that has been already published refers to the same patient but it is slightly different from this one.
PCR for Borrelia on tissue’s DNA (frozen or formalin-fixed and paraffin-embedded) can target OspA as reported by Cerroni (34), but also p41 (flagellin) and p66 (35). Skin biopsy specimens from the site of the lesion can also be submitted for culture and isolation of Borrelia.
Acrodermatitis Chronica Atrophicans (ACA)
ACA is the pathognomonic symptom of late LB. Patients, at presentation, should be asked whether they remember being bitten by a tick several months or even years before and whether they ever had an EM. Since the clinical appearance of ACA is not distinctive, it is of key importance to be generally alerted of the possibility of ACA in patients with bluish-red discoloration of a limb with or without swelling and/or atrophy, especially where LB is endemic (36, 37).
Unilateral acrocyanosis is present in the initial phases. This feature is followed by atrophy of the upper and/or lower limbs in an asymmetric manner, which, due to thinning and consequent greater transparency of the skin, allows the vessels of the dermis to be more visible. This condition leads over time to thinning of the most involved limb (22). ACA (Figure 5) is usually localized on the limbs, however, the face is also an acral site, and in some cases, it is difficult to distinguish the ACA of the face from Parry-Romberg syndrome, which may be a variant (38).

Acrodermatitis chronica atroficans of the legs.
In addition to ACA, in some cases, other atrophic-sclerodermic manifestations may be related to LB (39, 40).
Serology by chemiluminescence is usually very high in VlsE IgG; in Western-Blot, p93 (p83/100) and DbpA are generally observed.
Skin biopsy for histological examination and PCR for Borrelia are also possible for research purposes. Isolation of Borrelia in BSK medium from skin lesion can result in the growth of Borrelia afzelii (or more rarely valaisania, lusitaniae, or yangtze).
General and Extracutaneous Clinical Manifestations
General Symptoms
Important information to be obtained from patients includes: the geographical area where the patient lives (if endemic or not for LB), if, in the previous weeks or months the patient has been in wooded areas, if he/she has traveled or has been camping, or has spent time in public parks and gardens or if he/she owns any pets. Requested information should also include the date of the onset of symptoms, recollection of a tick bite and/or of a circular erythema as well as the location and the duration of the skin lesion. In the case of a positive, response, the patient should be asked if he/she was previously treated with antibiotics, what type of antibiotics, and what the duration of treatment was. Other clinical manifestations can be fever, lymphadenopathy, balance disorders, dizziness, and photophobia (44).
Joint and/or Muscular Symptoms
Arthritis occurs after 4 days to 2 years (average, 6 months) from EM (45–49). In a European group of patients, the period between the tick bite or EM to the onset of arthritis ranged from 10 days to 16 months, with an average of 3 months (50). A summary of the articular involvement of LB is reported in Table 1.
Table 1
Articular Involvement in LB.
| Features | Location | Clinic |
|---|---|---|
| Mono/Oligo Involvement | Large Joints | Swelling |
| Asymmetry frequent attacks | Knee Joint most affected | Marked functional Impotence |
| Skin Nodules | ||
| Absence of Stiffness in the Morning |
In the early phase, the patient presents mono- or oligoarticular migrant arthralgia at the level of the large joints. The first affected joint is often near the site of the EM or the tick bite. However, sometimes other large or small joints, such as the temporomandibular joint (TMA), are also affected (51). Over time, the duration of joint arthralgia tends to lengthen, while painless intervals become shorter.
The articular involvement in the late phase has different clinical features compared to the typical migrant myo-arthralgia of early LB. The clinical symptomatology is not easy to distinguish from arthritis due to other causes. The disorder can become chronic or intermittent, with attacks lasting from a couple of weeks to a few months, which can be followed by resolution of symptoms. The intensity of the attacks decreases over time. Hyperpyrexia is not usually present, but a general sense of fatigue is common.
Swelling of the joints with marked functional impotence is often present. Affected knees, for instance, may have very large effusions (synovial fluid) (52). If those injuries are not diagnosed and treated, the patient will possibly experience erosion of the cartilage and bone which can lead to permanent damage of the joint.
Muscular system involvement includes myalgia, muscle weakness, and myositis (53) with difficulty in raising the arms above the head, carrying weights, and climbing stairs; and dysphagia, with difficulty breathing due to the involvement of intercostal muscles (inter-costal diaphragm). In some cases, these symptoms can simulate a dermatomyositis (41).
To confirm diagnosis, it is useful to perform a serological ELISA test followed by a Western Blot. In case the patient reports having headaches and/or a fever, tests for TBE, Ehrlichia (Anaplasma), Rickettsia, and Bartonella coinfections are suggested. A rheumatologic examination can be also requested.
Serum IgG antibodies for B. burgdorferi s.l. are present in high titers in patients with Lyme arthritis, while a negative IgG serology rules out the diagnosis (54, 55). Serological investigation of synovial fluid is not helpful because of the absence of a blood–synovial barrier; IgG antibody concentration in serum and synovial fluid will be equivalent.
In some cases, it can be useful to perform a PCR for Borrelia using DNA from synovial fluid or from a biopsy fragment of the synovium (56).
If the clinical picture is suggestive of LB, but the serology is negative, the clinical symptoms should over-rule a negative test, as pointed out by Burgdorfer. Commercial test kits are often inaccurate and can give negative results even in advanced LB. A negative test does not demonstrate the absence of LB and further investigations are needed to rule out differential diagnoses, such as that for an autoimmune disease (57).
Neurological Symptoms
Involvement of the nervous system occurs in up to 15% of patients with untreated LB (58). A summary of the possible neurological manifestations in LB is reported in Table 2.
Table 2
Neurological Involvement in LB.
| Lymphocytic Meningitis | |
| Cranial neuritis | Facial palsy |
| Cranial nerves palsies of III, IV, VI | |
| Optic neuritis and optic atrophy | |
| Meningoradiculitis | Garin-Bujadoux-Bannwarth syndrome |
| Myelitis | Monofocal lesion |
| Multifocal lesions | |
| Acute transverse Myelitis | |
| Encephalitis | Loss of consciousness |
| Speech disorders | |
| Recent cognitive disorders | |
| Affective disorders | |
| Cerebral vasculitis | |
| Pseudo tumor cerebri | |
| Peripheral neuropathy | Chronic asymmetric neuropathy |
| Small fiber neuropathy | |
| Psychiatric disorders | States of anxiety |
| Depression | |
| States of panic |
Headache is the most frequent symptom. Cranial nerve involvement may occur, particularly that of the facial nerve (80%). Facial paralysis is bilateral in 25% (59, 60). Paralysis of the III, IV, VI cranial nerve, and optic neuritis can be observed.
Among children in Europe, the most common manifestations are facial nerve palsy (about 55%) and lymphocytic meningitis (about 30%) (61).
Meningopolyneuritis (Garin-Bujadoux-Bannwarth) with radicular pain and sometimes paresis of extremities or the abdominal wall (62, 63), neurologic bladder (64), and paresthesia can be observed. Myelitis is a rare manifestation of LB; although monofocal or multifocal lesions of the cervical spinal cord (65) have been described, as well as lombosacral myelitis (66) and acute transverse myelitis.
Pseudo tumor cerebri associated with LB was first described in 1985 (67). Subsequently, other cases have been described mainly in children (68) and rarely in adults (69).
Infection of the central nervous system is observed in 2–4% of Lyme neuroborreliosis, typically in the late or chronic stage of the disease (70). Encephalitis presents non-specific MRI findings of diffuse involvement of the brain parenchyma. Cerebral, cerebellar parenchyma, and thalami can be involved (71).
Neuroborreliosis can be associated with speech disorders, recent cognitive, and affective disorders (72), psychiatric disorders, states of anxiety, depression (73), and states of panic, and restless syndrome can be related to LB (74).
Cerebral vasculitis in patients with LB is observed in about 0.3% of cases (75). In some cases, the possibility of infection or co-infection (76) with Borrelia miyamotoi, which can be transmitted by the same tick as LB, should be considered (77, 78).
Neurological examination is suggested in order to rule out a differential diagnosis. In addition to the serological tests for anti-Borrelia antibodies by ELISA and Western Blot, it is also possible to perform a PCR for the detection of Borrelia DNA in cerebrospinal fluid (79) as well as an ELISA for Chemokine 13 (80).
Peripheral neuropathy can be detected in about 5–10% of Lyme neuroborreliosis cases. It can present as a chronic asymmetric neuropathy, usually without intrathecal antibodies (81).
For late neuroborreliosis, a careful examination is suggested for possible acrodermatitis chronica atrophicans (acral acrocyanotic appearance, and to verify any differences in limbs diameter) (82), and possibly a biopsy (for example on the ankle presenting neuropathic alterations) for histological examination of the small nervous fibers. Small fiber neuropathy (SFN) can be observed after antibiotic treatment (Post-treatment Lyme disease syndrome—PTLDS) and may be responsible for sensory symptoms (83).
In most patients, examination of the cerebrospinal fluid (CSF) reveals lymphocytic pleocytosis, damage to the blood-CSF-barrier, and an intrathecal synthesis of immunoglobulin IgM, IgG, and sometimes IgA (84); the protidorrachia is normal or slightly increased; the glycorrachia is normal or only slightly diminished.
During paralysis of the facial nerve, the CSF often presents lymphocytic pleocytosis even in the absence of signs and symptoms of meningitis (85).
After the onset of neurological symptoms, for a short time, intrathecal synthesis may not be detectable and CSF pleocytosis may be absent especially in children with isolated paralysis of the seventh cranial nerve (86). The production of intrathecal antibodies can continue even after recovery. On the other hand, intrathecal synthesis of specific antibodies is lacking in many patients with neuroborreliosis.
The use of chemokine (C–X–C motif) ligand 13 (CXCL13), a B-cell attracting chemokine, was debated for the laboratory diagnosis of acute Lyme neuroborreliosis in CSF (87). CXCL13 can be detected in CSF early in the disease and it has been reported to decrease with treatment (88). However, CXCL13 is not specific for Lyme neuroborreliosis and can also be found in some other inflammatory diseases of the CNS (88).
The different genospecies are often related to different clinical manifestations. Borrelia garinii is mainly related to typical early Lyme Neuroborreliosis (i.e., pain, meningoradiculoneuritis, or Bannwarth syndrome) while Borrelia valaisiana causes neurologic Lyme manifestations less frequently (89); Borrelia afzelii is less specific for neurologic manifestations as radicular pain and meningeal symptoms are rarely present (79). It is observed more often in late Neuroborreliosis by diffusion from the skin to small nerve fibers, often deriving from Acrodermatitis chronica atrophicans (82). It is able to cross the blood-brain barrier, but has a limited ability to produce inflammation in the CSF. The role of this genospecies has yet to be fully clarified.
Heart Symptoms
The involvement of the heart is observed in 4–10% of patients with LB, of whom 90% have Lyme carditis (90, 91). The most frequent manifestations are:
-
Atrioventricular Conduction disorder or other rhythm disorders,
-
Pericarditis (94),
-
Postural Orthostatic Tachycardia Syndrome (POTS) (95).
In addition to dyspnea, chest pain, or irregular heartbeat, typical symptoms include syncope episodes (93). On physical examination, 35% of patients had bradycardia and about 15% tachycardia.
If heart involvement in LB is suspected, a cardiological examination is suggested. The following investigations should be addressed: 12-channel ECG and 24-h ECG Holter (query: rhythm analysis, PQ interval, QRS width, ectopic beats), chest X-ray (question: heart size, congestion); echocardiography (diameter, ejection fraction, abnormal wall movement, pericardial effusion); cardiac MRI, and in selected cases myocardial biopsy for histological examination and cultural isolation of Borrelia (96). Electrophysiological examination can be done only in selected cases to confirm the diagnosis and establish a prognosis, as it is a highly invasive procedure and can cause arrhythmia. Patients should be clearly informed about the procedure and its associated risk.
Ocular Symptoms
Ocular manifestations can be linked to a direct involvement of the eye or can be secondary to Neuroborreliosis. Ocular involvement, is possible at every stage of LB and they can be summarized as follows:
-
Follicular conjunctivitis often self-limited, and,
-
Photophobia.
They can appear in the first stages of LB.
In the early disseminated phase, these manifestations are possible:
-
Macular edema,
-
Uveitis and Iridocyclitis,
-
Optic Neuritis and Neuroretinitis,
-
Retinal Vasculitis and Choroiditis,
-
Branch Retinal Vein Occlusion (BRVO) (97),
-
White Dot Syndrome (98),
-
Stromal Keratitis and Episcleritis.
Intermediate uveitis is the most common uveitis in LB. Posterior uveitis is mostly associated with chorioretinal involvement (99).
Keratitis is characteristic of the second and third stages of LB and may either be interstitial or ulcerative. Episcleritis and scleritis are rare and can be observed mainly in the late phase of LB (100).
Regarding ocular manifestations due to Neuroborreliosis, they include:
When to Suspect Coinfections
Coinfections should be suspected in the following cases (103, 104):
-
✓ in the presence of fever and headache,
-
✓ in patients diagnosed with LB, who do not clinically improve or,
-
✓ whose symptoms have changed (e.g., appearance of febrile episodes) after adequate antibiotic treatment,
-
✓ when patients have leukopenia and neutropenia, persistent after treatment, or high ESR,
-
✓ when patients present purple, persistent skin lesions, even the same purpuric Erythema migrans (in our experience).
In these cases tests for Rickettsia, Anaplasma (105), Bartonella, Babesia (106), and TBE (FSME Frühsommer-Meningoenzephalitis) (105, 107) and Powassan virus (108) are suggested.
Occasional Positivity of Anti-Borrelia Antibodies
The spirochetes may persist in affected organs even months to years after the initial infection, causing a chronic form of illness. Therefore, antimicrobial agents have been found to have a role in all stages of the disease (109).
When patients come to the Lyme Disease Center, because they have been found to be positive for anti-Borrelia antibodies, it is necessary to request an accurate medical history including the geographical area where the patient lives, recollection of a tick bite, and if applicable, the recollection of a circular rash, its possible location, and its duration. This collection of information should be followed by an accurate examination for the presence of LB related symptoms. Medical history should also include any previous antibiotic treatment.
In the absence of any reported tick bite or EM and related clinical manifestations, if the serological test results are positive in IgG antibodies it is recommended to perform a WB, whereas positive IgM may not be specific, and serology should be repeated after 6 months.
When the skin, the myo-articular system, and/or the nervous, cardiac or ocular systems are involved, specific investigations must be carried out, as indicated in the two previous paragraphs.
These patients should also be subjected to immunological testing, as Borrelia antigens can induce autoimmune diseases in predisposed subjects (Trigger Factor).
In some cases, Borrelia induces the production of antibodies against certain surface antigens, which cross-react with specific sequences of organism structures (antigenic camouflage). It is known, in fact, that there can be cross-reactivity between OspA and the human leukocyte function antigen (LFA) (110, 111), as well as between Osp and acetylcholine receptors, enolase gamma, and Borrelia Enolase (112).
A thorough diagnostic examination should be based on the clinical picture, the organs involved, the serological pattern, and the tests that have been already performed.
Persistence of the Clinical Manifestations after Treatment
The persistence of symptoms related to LB can be observed in untreated patients as well as in patients who have undergone treatment but continue to present symptoms. Untreated patients can develop persistent signs and symptoms, which usually involve the joints and less commonly the nervous system (113). Patients who instead have been treated mainly report a worsening of subjective symptoms. After 6 months, 36% of patients experienced an increase in fatigue, 20% complained of widespread pain, and 45% of neurocognitive impairment (114). Long-term persistent illness following antibiotic treatment is not uncommon, especially when treatment is delayed. About 10–20% of patients treated for early or late LB experience persistent symptoms, which may last for months or years (115). Symptoms consist of fatigue, joint and muscle pains, recent cognitive disorders, root pain, paresthesia, or dysesthesia. If we analyze the group of patients treated for Neuroborreliosis, this percentage increases significantly. Eikeland found that in Europe only 56% of patients treated with antibiotics for neuroborreliosis were symptom-free 30 months after treatment (116, 117).
Some published authors of medical research recognize mainly two clinical scenarios: the first characterized by typical symptoms of post-Lyme disease when symptoms persist for <6 months, and post-treatment Lyme disease syndrome or chronic Lyme disease if symptoms are debilitating and persist after treatment (118).
In the International Lyme and associated diseases society (ILADS) guidelines, “chronic Lyme disease” is described as a multisystem illness with persistent symptoms (119, 120), including fatigue, cognitive dysfunction, headaches, sleep disturbances, and other neurologic features, such as demyelinating disease, peripheral neuropathy, and sometimes motor neuron disease, neuropsychiatric presentations, cardiac presentations (including electrical conduction delays and dilated cardiomyopathy), and musculoskeletal problems (121–123). The cause may consist in residual damage to tissues and the immune system and cytokine production (122, 123), which occurs as a consequence of the infection causing possible modification of protein antigens located on the cell membrane. According to certain controlled studies, post-treatment Lyme disease syndrome (PTLDS) has often been shown to be non-responsive to antibiotic therapy. Several hypotheses have been suggested in order to explain PTLDS, among them, the presence of bacterial debris, autoimmunity, and co-infections, (120, 124, 125). In several studies, persistent Borrelia was isolated by culture or PCR (126–139).
The effectiveness of Ceftriaxone in several cases supports the hypothesis of bacterial persisters which survive in spite of previous antibiotic treatment (140). Delong et al. (140) have reported that retreatment can be effective, but further studies are needed to assess the role of antibiotics for persistent infection. It has been demonstrated that the persistence of Borrelia burgdorferi is likely due to the development of biologically less active permanent forms (Spheroblasts and round shapes) and of biofilm (141, 142). Biofilm analysis (Clinical Biofilm Ring Test—cBRT) (143) and treatment can produce an improvement in test results (144). In some cases, Borrelia can induce the production of antibodies against certain surface antigens, which cross-react with specific sequences of organism structures (antigenic camouflage). OspA is known, in fact, to cross-react with LFA, as well as Osp with Acetylcholine receptors. Treatment of B. burgdorferi in the stationary phase can result in a higher probability of regrowth once antibiotic treatment is interrupted (119).
Post-Treatment Lyme Disease Symptoms (PTLDS) and Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME) have several clinical features in common, including fatigue, musculoskeletal pain, and cognitive difficulties. The Canadian Clinical Criteria for CFS/ME diagnosis include the following symptoms: Fatigue > 6 months, limited physical activity, unrefreshing sleep, impaired thinking and speech, vertigo, post-exertional fatigue, stress induced by exertion, reduced concentration, orthostatic intolerance, food intolerance (145).
Immunologic mechanisms have been suspected to play a role in both PTLDS and CFS/ME.
In CFS/ME patients, serum Activin B levels were significantly elevated compared with control subjects. Elevated Activin B levels together with normal Activin A levels identified patients with the diagnostic symptoms of CFS/ME (146, 147).
It has also been hypothesized that there is an immunosignature specific to CFS/ME and that this could aid the diagnosis. Scientists were in fact able to identify a 256-peptide signature that separates CFS/ME samples from healthy controls (148).
An increase in levels and frequency of IgG anti-neural antibody reactivity has been found in PTLDS. The anti-neural antibody response was independent from serologic positivity for antibodies to Borrelia burgdorferi; however there was no significant difference in the prevalence of anti-neural antibody reactivity between CFS/ME patients and healthy controls (149).
Pregnancy and Pediatric Case Assessment
It is documented that trans-placental transmission of the spirochetes from the mother to the fetus is possible, and Borrelia starts crossing the placenta (150, 151) during the first month, unlike Treponema, which passes through the placenta barrier starting from the 5th month. A case of congenital Lyme with multiple annular erythema at birth has been reported in a child whose mother reported having an erythema migrans during pregnancy. Culture of skin biopsy from the child‘s skin lesion was positive for Borrelia garinii and rapid recovery was achieved after antibiotic therapy (152). A study on seven pregnant European women with EM and Borrelia isolated from blood indicated that the course and outcome of early LB was uneventful when pregnant women were treated with intravenous ceftriaxone, and that the outcome of their pregnancies was good (153). Therefore, in case of pregnancy, antibiotic prophylaxis treatment may be appropriate in the case of tick bites in endemic areas.
Below is a description of the symptoms of LB in children with potential exposure to tick bites, who have been diagnosed with EM or positive serological results or clinical manifestations compatible with LB.
Clinical suspicion of Lyme disease is based on the following clinical manifestations: for early localized LB, the presence of erythema migrans, often on the face, possibly associated with conjunctivitis and/or photophobia; for early disseminated LB the presence of multiple annular erythemas, Borrelial lymphocytoma, cranial neuritis, headache and/or pain and stiffness in the neck, migrant myo-arthralgia with possible involvement of the temporomandibular joint, alterations of electrocardiogram suggestive of carditis; for late BL the presence of arthritis. Acrodermatitis chronica atrophicans can also occur in children, but it is rare (154).
Patients with non-specific symptoms (e.g., fever or fatigue without specific manifestations of early, disseminated or late Lyme disease) are classified as probably not affected by Lyme disease. These patients should be considered positive only if, after 1 month, serology tests demonstrate serum conversion.
In some cases a rapid test response is required, ELISA or CLIA (155). Clinical evaluation plays a fundamental role when having to make initial decisions regarding children who visit the pediatric emergency room.
Detection of Borrelia in Clinical Samples
Indirect Methods of Borrelia Detection
Detection of Antibodies Against Borrelia burgdorferi sensu lato Complex
Several commercial products are available for detecting IgG and/or IgM antibodies against Borrelia burgdorferi s.l. complex. Test systems comprise different techniques including the Enzyme-linked immunosorbent assay (ELISA), the Enzyme-Immunoassay (EIA), the Enzyme-Linked Fluorescence Assay (ELFA), the Chemoluminescence Immunoassay (CLIA), Luminex, Fluoro-Immunoassay (FIA), and Western Blots/Immunoblots. Some tests use antigens obtained from native Borrelia bacteria, whilst others use manufacturing methods to prepare recombinant antigens. In some assays a mixture of both are used.
The European and North American guidelines indicate that the diagnosis of LB is currently based on a two-tier serology at all stages of the infection, except when erythema migrans is present (156). The two-tier testing procedure includes ELISA or EIA or VlsE/C6 as the first test and a Western Blot/Immunoblot assay as a confirmatory test. The VlsE Complex (variable major protein-like sequence Expressed—Vmp 35 kDa) is a surface protein formed by three defined domains: two invariable constant regions at the COOH and NH2 terminals, and one internal variable region. The invariable, internal areas are masked and protected by the “in vivo” external variable regions. Due to the continuous modifications of its external antigenically variable component, Borrelia is able to escape the immune system.
After the death of the spirochetes, the VlsE protein is presented in its entirety to the immune system, which can thus induce the production of antibodies against the preserved and invariable regions of VlsE. The dosage of the VlsE protein and its sixth invariant region (IR6) peptide of Borrelia burgdorferi has been reported to quantitatively vary after antibiotic treatment (157–159), although VlsE and C6 are detected both in convalescent and healthy people, and thus they do not differentiate between active and past infection. OspC is used for detection of specific IgM antibodies in the first stage of the serologic test, either as a single antigen or as a mixture with other antigens.
Immunoblot (western blot) is generally used to confirm positivity and can characterize the immune responses to specific proteins of Borrelia burgdorferi s.l. complex. The test kit manufacturers clearly define the interpretation for positive, negative, and equivocal samples.
The European Union Concerted Action on Lyme Borreliosis/EUCALB has conducted a multicenter study for the standardization of the interpretative criteria of immunoblot results in Europe. Although a set of eight bands were identified as significant in each participant laboratory, no single rule was formulated for use across Europe (160). The sensitivity of serological tests for diagnosis of LB is highly heterogeneous, varying with clinical manifestations (161). Average sensitivity estimates of 50% for erythema migrans, 77% for neuroborreliosis, 97% for acrodermatitis chronica atrophicans, and 73% for unspecified LB have been reported (162). Overall, the mean sensitivity of the serologic test was reported in a meta-analysis to be 59.5% (range: 30.6–86.2%) (163). Most European and North American guidelines recommend searching for intrathecal antibody production for the diagnosis of early Lyme neuroborreliosis (156).
In recent years, other commercially available serological tests have been developed for Borrelia detection. Among them, the TickPlex assay is an ELISA-based test, which also contains a new antigen for round bodies/persister forms of Borrelia. This assay has been reported to be useful in different stages of LB and the upgraded test also allows to simultaneously determine IgM and IgG antibodies of several tick-transmitted bacterial and viral pathogens (https://www.arminlabs.com/en/tests/tickplex).
Direct Detection of Borrelia
Direct detection of B. burgdorferi sensu lato can be achieved by culture of the infectious agent, by microscopy, and by the use of molecular methods for the detection of Borrelia nucleic acids. These methods vary in sensitivity and procedure complexity. They can provide evidence for the presence of intact spirochetes or spirochete components, such as DNA or protein, in tick vectors, reservoir hosts, or patients.
Culture
Although in vitro cultivation of Borrelia from clinical samples represents the golden standard for proving an active infection, this method cannot be routinely used for diagnosis as it is time consuming and has low clinical sensitivity (54, 164). Borrelia burgdorferi sensu lato culture can be obtained from various tissues and body fluids with variable yield using dedicated media, such as the modified Kelly-Pettenkofer medium (MKP), the Barbour-Stoenner-Kelly II (BSK-II) medium, and the commercially available BSK-H medium (165, 166). Borrelia cultivation from clinical samples is mostly successful from skin biopsy when compared to blood and CSF cultures (165, 167).
Microscopy
Borrelia burgdorferi sensu lato detection by light microscopy is not feasible in clinical practice. The low Borrelia load does not allow a direct recognition of the spirochetes in tissue slides for routine diagnostic procedures. However, for specific purposes, the Warthin-Starry’s silver stain (168, 169) and more recently the focus floating microscopy (FFM) (170–173), which are light microscopy-based techniques, can be used to detect Borrelia in clinical tissues. In addition, Borrelia species were also detected by electron microscopy in human samples from myocardial tissues (174) and crystalline keratopathy (175).
PCR
Among molecular methods of detecting Borrelia‘s nucleic acids, PCR-based methods are the most widely used for confirmation of Borrelia infection (167). However, Borrelia diagnosis continues to be very difficult, even by PCR (176). PCR sensitivity for Borrelia diagnosis is, indeed, highly variable, because of the multiple factors involved in its detectability by PCR. The type of starting material (blood, skin biopsies, cerebrospinal fluid, synovial fluid), the DNA extraction protocols, the possible use of systems for enrichment of microbial DNA, the PCR targets and PCR approach (nested PCR, real time PCR, digital PCR, PCR followed by hybridization, etc.) influence PCR sensitivity (167, 177, 178). The variability in specimens mentioned above and target amplification have also been found in the CE-IVD PCR assays developed for Borrelia detection (177). Low bacterial concentration is the main concern, and a further hypothesis regarding the possibility that during infection Borrelia invades the intracellular niche has been suggested (176). Moreover, different non-motile atypical morphologies of B. burgdorferi (s.l.) spirochetes have been reported. These include looped or ring-shaped forms, blebs, round bodies, and cell wall deficient forms; spirochete colonies or biofilm aggregates have also been described. The above-mentioned morphologies can impact Borrelia detectability by PCR. Biofilm busters to increase Borrelia load have been suggested for more accurate PCR tests (144). Borrelia PCR from skin biopsy from patients with ECM and ACA usually has a higher rate of positivity, but with large variation among studies (167). However, as the lesions are per se pathognomonic of LB, PCR is now only used for research purposes for those lesions. The diagnostic sensitivity of PCR in body fluids is highly variable, depending on the sample type, on the volume of the sample and on the contamination from PCR inhibitors (179). In synovial fluid, PCR for Borrelia detection is more sensitive than in blood and CSF (167). Borrelia targets for PCR must be genetically stable and should enable the detection of all pathogen of Borrelia species. They can be located on the chromosome or on plasmid DNA. The most frequent chromosomal targets that have been reported in clinical studies are flagellin (26, 164, 180–182), 16S rRNA gene (180, 183–185), the gene codifying for the 66 kDa protein (26, 56, 184, 185), while the most used plasmid target is OspA (56, 180, 183, 186–188), which has been also reported to be more stable after degradation of spirochetes (178). At present the major concern in Borrelia diagnosis by PCR is the lack of standardization of the protocols and analyzed targets (167, 177, 178). This heterogeneity in terms of PCR protocols and samples makes it difficult to diagnose LB unequivocally by PCR in settings in which the pre-test probability of LB is very low, including for instance patients suspected of late LB, with negative serology (178).
Novel Approaches in Borrelia Detection
Because of the limits of serology in detecting the Borrelia sensu lato complex in clinical samples, other commercially available tests have been developed. Among them, the T cell response tests, including the lymphocyte transformation test (LTT and MELISA) and the enzyme linked immuno-spot (EliSpot) test have been commercialized. They are based on the detection in patients’ blood of Borrelia-specific T-lymphocyte, notably the T helper lymphocytes, which are reported to circulate in the blood in detectable numbers only during an active immune response against Borrelia and to persist in a non-florid infection in lymphoid organs (189).
Alternative tests to the traditional serology and PCR for Borrelia detection have also been proposed. Among them, Luminex-based approaches for Borrelia detection have been reported. This multiplex- high-throughput technique was used for the simultaneous detection of the plasmid contents of different B. burgdorferi strains (10 Ag-Luminex technology) (190), but also to diagnose Borrelia miyamotoi in the serum of European patients (191) as well as for the simultaneous detection of 10 insect-borne pathogens, including Borrelia (192). An immuno-PCR (iPCR) assay, which takes advantage of the PCR properties to increase the sensitivity of standard ELISA (193), was also developed and evaluated for the detection of antibodies to the B. burgdorferi C6 peptide (194). Other approaches refer to the metabolic profiling for early Lyme disease (195) and the measurement of IFN-γ after incubating blood with Borrelia antigens. The latter method was reported to be potentially useful in the laboratory diagnosis of early Lyme disease, even after antibiotic treatment (196).
Ethics Statement
Written informed consent was obtained as part of the hospital procedures from the individuals and/or minor’ legal guardian/next of kin for the publication of any potentially identifiable images included in this article.
Author Contributions
GT managed the clinical aspect of the review, MR the section dedicated to serology, SB the section related to direct diagnosis go LB. All authors drafted and revised the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Erica Falkingham for the language revision of the manuscript and the Associazione Lyme Italia e Conifezioni for supporting Lyme Borreliosis studies and dissemination.
References
https://forskning.no/sykdommer-insekter/slik-kan-flattbitt-gi-deg-kjottallergi/423258

Slik kan flåttbitt gi deg kjøttallergi
Det ser ut til at et flåttbitt for noen kan bety slutten på å spise koteletter og biff for alltid. Men hvordan kan dette henge sammen?
De seneste årene har forskere avdekket av flåttbitt kan gi livslang kjøttallergi.
Ifølge svenske forskere, som har gjort en studie på dette, er det oppdaget stadig flere tilfeller av nettopp denne allergien i Sverige de siste årene, ifølge Astma- og allergiforbundet.
Her har vi spurt noen eksperter hvordan flåttbitt og kjøttallergi kan kobles sammen.
Nylig oppdaget form for allergi
– Ett bitt er antakelig alt som skal til for å utvikle slik kjøttallergi.
Det sier allergiforsker Allan Linneberg. Han er klinisk professor ved Københavns Universitet og Forskningscenter for Forebyggelse og Sundhed og Rigshospitalet.
Har du først fått kjøttallergi, må du holde deg unna storfe, lam, vilt og svinekjøtt resten av livet hvis du vil unngå potensielt voldsomme allergiske reaksjoner.
Reaksjonene kan være mageproblemer, utslett over hele kroppen og i verste fall allergisk sjokk med livstruende lavt blodtrykk.
forskning.no skrev i 2010 en artikkel om kjøttallergi, som tydet på at det da var svært få som var plaget av dette her i landet. Det er uvisst om tallet har steget.
Kjøttallergi ble først oppdaget for omtrent fem år siden, og de siste årene har flere studier koblet allergien sammen med flåttbitt.
- Les også: Kan man bli allergisk mot kjøtt?
Flåttens bedøvelse setter gang i allergien
Allergien kickstartes antagelig når flåtten borer munnen og hodet sitt ned under huden din for å suge blod.
I samme prosess sprøyter den inn litt væske under huden for å bedøve og for å undertrykke immunforsvaret.
– Den lager et hull i overhuden – den bruker enzymer til å løse den opp og så lager den et hulrom i huden som blodet samles i, og som den kan spise fra, beskriver flåttforsker og førsteamanuensis ved Institut for Plante- og Miljøvidenskab ved Københavns Universitet, Per Moestrup Jensen.
- Les også: – Vi vet for lite om flått
I bedøvelsesvæsken finnes sannsynligvis også et lite sukkermolekyl ved navn a-Gal, som aktiverer immunforsvaret og kan sette i gang kjøttallergien.
Dette molekylet er ufarlig for kroppen, men immunforsvaret oppfatter det antakelig som en fiende og danner antistoffer mot det.
Antistoffene gjør at neste gang immunforsvaret oppdager a-Gal, vil det sette i gang en allergisk reaksjon i hele kroppen.
Det kan for eksempel være når du setter tennene i en stor, saftig biff.
a-Gal finnes nemlig også i storfekjøtt, lammekjøtt, hjortekjøtt og svinekjøtt.
- Les også: Egg mot eggallergi
Hvorfor får vi ikke allergi fra a-Gal i kjøtt?
Selv om du altså får massevis av a-Gal inn i kroppen via kjøttet, kan du ikke få kjøttallergi av å spise kjøtt.
Det er antakelig fordi du får det i deg i store mengder i løpet av måltidet og at det kommer inn i fordøyelsessystemet, som gjør at immunforsvaret ikke reagerer.
– Men når du får det sprøytet inn gjennom huden i veldig små doser, så vil immunforsvaret oppfatte molekylet annerledes. Forsvaret aktiveres og da har skaden kanskje skjedd, sier Allan Linneberg.
Per Moestrup Jensen har påvist at flåttens magesekk inneholder rester av blod fra de dyrene den har sugd blod fra.
Derfor kan a-Gal-molekylene kanskje stamme fra det dyret som var blodsugerens tidligere vert.
– Vi kan ikke utelukke at det kan skje en overføring av molekyler fra vert til vert. Det å få molekyler som er beslektet med kjøtt, rett inn i blodet, vil med stor sannsynlighet kunne starte en reaksjon i immunforsvaret vårt, sier han.
Han undrer seg imidlertid over hvordan innholdet fra flåttens magesekk ender opp i spyttkjertlene dens og dermed i den nye verten.
– Det krever at de kaster opp. Det er det en enkelt studie som viser at de kan, men dokumentasjonen for det er ganske svak, understreker han.
- Les også: Blir vi syke av norsk kjøtt?
Oppdagelsen av kjøttallergi startet som en detektivhistorie
Både kjøttallergi i seg selv og flåttenes rolle i utviklingen av den ble oppdaget ved en tilfeldighet, forteller Linneberg.
Amerikanske leger på et kreftsykehus stusset i begynnelsen av 2000-tallet over at noen av pasientene deres reagerte allergisk overfor en bestemt type medisiner som var utviklet med komponenter fra mus.
De fant ut at pasientene var allergiske overfor a-Gal, som finnes i mus og dermed i denne kreftmedisinen.
De syntes det var rart at en del pasienter reagerte allergisk første gang de fikk medisinen.
En allergisk reaksjon starter nemlig først hvis immunforsvaret har møtt det allergifremkallende stoffet tidligere og dannet antistoffer mot det.
Så hvordan hadde immunforsvaret hos de kreftsyke dannet antistoffer mot a-Gal når det var første gang de fikk medisinen?
– Det er jo litt av en detektivhistorie, dette her, sier Linneberg.
- Les også: Er rødt kjøtt virkelig så farlig?
Kjøttallergi kobles til flåttbitt
En gruppe forskere fra University of Virginia fant siden ut at det var geografisk betinget hvilke pasienter som var allergiske mot a-Gal.
I bestemte geografiske områder var det både en høy forekomst av en spesiell flåttart og av en mystisk kjøttallergi.
Forskerne intervjuet 24 pasienter som alle hadde antistoffer mot a-Gal.
Samtlige pasienter hadde opplevd symptomer på allergisk sjokk med høy puls og pusteproblemer etter at de hadde spist kjøtt.
Flere av kreftpasientene hadde opplevd lignende reaksjoner. Dermed ble a-Gal og kjøttallergi koblet sammen.
I 2013 klarte svenske forskere fra Karolinska Instituttet å koble flått og kjøttallergi enda tettere sammen.
De påviste nemlig at a-Gal-molekylet finnes i flåttens mage.
Samtidig undersøkte de 50 pasienter med kjøttallergi. Alle hadde vært vert for en flått før allergien startet.
De svenske forskerne mener det er sannsynlig at stadig flere vil risikere å utvikle allergi mot rødt kjøtt på grunn av flåttbitt. Dette fordi flåtten i Sverige øker i utbredelse som følge av stadig flere stammer med rådyr og gnagere som er vertskap for flåtten.
Og det er så langt forskningen for øyeblikket har kommet i avsløringen av rollen de små blodsugerne spiller i utviklingen av kjøttallergi.
Referanser:
S.P Commins mfl: Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. Journal of Allergy and Clinical Immunology, 2009. Sammendrag.
M. Starkhammar og M. Van Hage: Fästingbett kan leda till utveckling av köttallergi. Allergi i praxis, 2013.
© Videnskab.dk. Oversatt av Marianne Nordahl for forskning.no.
Borrelia burgdorferi – en unik bakterie
Øystein Brorson Om forfatteren
IJGM-75825-clinical-determinants-of-lyme-borreliosis--babesiosis--barto_122314
Lyme disease
Jump to navigationJump to search
| Lyme disease | |
|---|---|
| Other names | Lyme borreliosis |
 |
|
| An adult deer tick (most cases of Lyme are caused by nymphal rather than adult ticks) | |
| Specialty | Infectious disease |
| Symptoms | Expanding area of redness at the site of a tick bite, fever, headache, tiredness[1] |
| Complications | Facial nerve paralysis, arthritis, meningitis[1] |
| Usual onset | A week after a bite[1] |
| Causes | Borrelia spread by ticks[2] |
| Diagnostic method | Based on symptoms, tick exposure, blood tests[3] |
| Prevention | Prevention of tick bites (clothing the limbs, DEET), doxycycline[2] |
| Medication | Doxycycline, amoxicillin, ceftriaxone, cefuroxime[2] |
| Frequency | 365,000 per year[2][4] |
Lyme disease, also known as Lyme borreliosis, is an infectious disease caused by the Borrelia bacterium which is spread by ticks.[2] The most common sign of infection is an expanding red rash, known as erythema migrans, that appears at the site of the tick bite about a week after it occurred.[1] The rash is typically neither itchy nor painful.[1] Approximately 70–80% of infected people develop a rash.[1] Other early symptoms may include fever, headache and tiredness.[1] If untreated, symptoms may include loss of the ability to move one or both sides of the face, joint pains, severe headaches with neck stiffness, or heart palpitations, among others.[1] Months to years later, repeated episodes of joint pain and swelling may occur.[1] Occasionally, people develop shooting pains or tingling in their arms and legs.[1] Despite appropriate treatment, about 10 to 20% of people develop joint pains, memory problems, and tiredness for at least six months.[1][5]
Lyme disease is transmitted to humans by the bites of infected ticks of the genus Ixodes.[6] In the United States, ticks of concern are usually of the Ixodes scapularis type, and must be attached for at least 36 hours before the bacteria can spread.[7][8] In Europe, ticks of the Ixodes ricinus type may spread the bacteria more quickly.[8][9] In North America, the bacteria Borrelia burgdorferi and Borrelia mayonii cause Lyme disease.[2][10] In Europe and Asia, Borrelia afzelii and Borrelia garinii are also causes of the disease.[2] The disease does not appear to be transmissible between people, by other animals, or through food.[7] Diagnosis is based upon a combination of symptoms, history of tick exposure, and possibly testing for specific antibodies in the blood.[3][11] Blood tests are often negative in the early stages of the disease.[2] Testing of individual ticks is not typically useful.[12]
Prevention includes efforts to prevent tick bites such as by wearing clothing to cover the arms and legs, and using DEET or picaridin-based insect repellents.[2] Using pesticides to reduce tick numbers may also be effective.[2] Ticks can be removed using tweezers.[13] If the removed tick was full of blood, a single dose of doxycycline may be used to prevent development of infection, but is not generally recommended since development of infection is rare.[2] If an infection develops, a number of antibiotics are effective, including doxycycline, amoxicillin, and cefuroxime.[2] Standard treatment usually lasts for two or three weeks.[2] Some people develop a fever and muscle and joint pains from treatment which may last for one or two days.[2] In those who develop persistent symptoms, long-term antibiotic therapy has not been found to be useful.[2][14]
Lyme disease is the most common disease spread by ticks in the Northern Hemisphere.[15] It is estimated to affect 300,000 people a year in the United States and 65,000 people a year in Europe.[2][4] Infections are most common in the spring and early summer.[2] Lyme disease was diagnosed as a separate condition for the first time in 1975 in Old Lyme, Connecticut.[16] It was originally mistaken for juvenile rheumatoid arthritis.[16] The bacterium involved was first described in 1981 by Willy Burgdorfer.[17] Chronic symptoms following treatment are well described and are known as “post-treatment Lyme disease syndrome” (PTLDS).[14] PTLDS is different from chronic Lyme disease, a term no longer supported by the scientific community and used in different ways by different groups.[14][18] Some healthcare providers claim that PTLDS is caused by persistent infection, but this is not believed to be true because no evidence of persistent infection can be found after standard treatment.[19] A vaccine for Lyme disease was marketed in the United States between 1998 and 2002, but was withdrawn from the market due to poor sales.[2][20][21] Research is ongoing to develop new vaccines.[2]
Signs and symptoms[edit]
An expanding rash is an initial sign of about 80% of Lyme infections. The rash may look like a “bull’s eye”, as pictured, in about 80% of cases in Europe and 20% of cases in the US.[22][23][24][25]
Lyme disease can affect multiple body systems and produce a broad range of symptoms. Not everyone with Lyme disease has all of the symptoms, and many of the symptoms are not specific to Lyme disease but can occur with other diseases as well.
The incubation period from infection to the onset of symptoms is usually one to two weeks, but can be much shorter (days), or much longer (months to years).[26] Lyme symptoms most often occur from May to September in the northern hemisphere, because the nymphal stage of the tick is responsible for most cases.[26] Asymptomatic infection exists, but occurs in less than 7% of infected individuals in the United States.[27] Asymptomatic infection may be much more common among those infected in Europe.[28]
Early localized infection[edit]
Early localized infection can occur when the infection has not yet spread throughout the body. Only the site where the infection has first come into contact with the skin is affected. The initial sign of about 80% of Lyme infections is an Erythema migrans (EM) rash at the site of a tick bite, often near skin folds, such as the armpit, groin, or back of knee, on the trunk, under clothing straps, or in children’s hair, ear, or neck.[22][2] Most people who get infected do not remember seeing a tick or the bite. The rash appears typically one or two weeks (range 3–32 days) after the bite and expands 2–3 cm per day up to a diameter of 5–70 cm (median 16 cm).[22][2][23] The rash is usually circular or oval, red or bluish, and may have an elevated or darker center.[2][24][25] In about 79% of cases in Europe but only 19% of cases in endemic areas of the U.S., the rash gradually clears from the center toward the edges, possibly forming a “bull’s eye” pattern.[23][24][25] The rash may feel warm but usually is not itchy, is rarely tender or painful, and takes up to four weeks to resolve if untreated.[2]
The EM (Erythema migrans) rash is often accompanied by symptoms of a viral-like illness, including fatigue, headache, body aches, fever, and chills, but usually not nausea or upper-respiratory problems. These symptoms may also appear without a rash, or linger after the rash disappears. Lyme can progress to later stages without these symptoms or a rash.[2]
People with high fever for more than two days or whose other symptoms of viral-like illness do not improve despite antibiotic treatment for Lyme disease, or who have abnormally low levels of white or red cells or platelets in the blood, should be investigated for possible coinfection with other tick-borne diseases, such as ehrlichiosis and babesiosis.[29]
Early disseminated infection[edit]
Within days to weeks after the onset of local infection, the Borrelia bacteria may spread through the lymphatic system or bloodstream. In 10–20% of untreated cases, EM rashes develop at sites across the body that bear no relation to the original tick bite.[22] Transient muscle pains and joint pains are also common.[22]
In about 10–15% of untreated people, Lyme causes neurological problems known as neuroborreliosis.[30] Early neuroborreliosis typically appears 4–6 weeks (range 1–12 weeks) after the tick bite and involves some combination of lymphocytic meningitis, cranial neuritis, radiculopathy and/or mononeuritis multiplex.[29][31] Lymphocytic meningitis causes characteristic changes in the cerebrospinal fluid (CSF) and may be accompanied for several weeks by variable headache and, less commonly, usually mild meningitis signs such as inability to flex the neck fully and intolerance to bright lights, but typically no or only very low fever.[32] In children, partial loss of vision may also occur.[29] Cranial neuritis is an inflammation of cranial nerves. When due to Lyme, it most typically causes facial palsy impairing blinking, smiling, and chewing in one or both sides of the face. It may also cause intermittent double vision.[29][32] Lyme radiculopathy is an inflammation of spinal nerve roots that often causes pain and less often weakness, numbness, or altered sensation in the areas of the body served by nerves connected to the affected roots, e.g. limb(s) or part(s) of trunk. The pain is often described as unlike any other previously felt, excruciating, migrating, worse at night, rarely symmetrical, and often accompanied by extreme sleep disturbance.[31][33] Mononeuritis multiplex is an inflammation causing similar symptoms in one or more unrelated peripheral nerves.[30][29] Rarely, early neuroborreliosis may involve inflammation of the brain or spinal cord, with symptoms such as confusion, abnormal gait, ocular movements, or speech, impaired movement, impaired motor planning, or shaking.[29][31]
In North America, facial palsy is the typical early neuroborreliosis presentation, occurring in 5–10% of untreated people, in about 75% of cases accompanied by lymphocytic meningitis.[29][34] Lyme radiculopathy is reported half as frequently, but many cases may be unrecognized.[35] In European adults, the most common presentation is a combination of lymphocytic meningitis and radiculopathy known as Bannwarth syndrome, accompanied in 36-89% of cases by facial palsy.[31][33] In this syndrome, radicular pain tends to start in the same body region as the initial erythema migrans rash, if there was one, and precedes possible facial palsy and other impaired movement.[33] In extreme cases, permanent impairment of motor or sensory function of the lower limbs may occur.[28] In European children, the most common manifestations are facial palsy (in 55%), other cranial neuritis, and lymphocytic meningitis (in 27%).[31]
In about 4–10% of untreated cases in the U.S. and 0.3–4% of untreated cases in Europe, typically between June and December, about one month (range 4 days-7 months) after the tick bite, the infection may cause heart complications known as Lyme carditis.[36][37] Symptoms may include heart palpitations (in 69% of people), dizziness, fainting, shortness of breath, and chest pain.[36] Other symptoms of Lyme disease may also be present, such as EM rash, joint aches, facial palsy, headaches, or radicular pain.[36] In some people, however, carditis may be the first manifestation of Lyme disease.[36] Lyme carditis in 19–87% of people adversely impacts the heart’s electrical conduction system, causing atrioventricular block that often manifests as heart rhythms that alternate within minutes between abnormally slow and abnormally fast.[36][37] In 10–15% of people, Lyme causes myocardial complications such as cardiomegaly, left ventricular dysfunction, or congestive heart failure.[36]
Another skin condition, found in Europe but not in North America, is borrelial lymphocytoma, a purplish lump that develops on the ear lobe, nipple, or scrotum.[38]
Late disseminated infection[edit]
After several months, untreated or inadequately treated people may go on to develop chronic symptoms that affect many parts of the body, including the joints, nerves, brain, eyes, and heart.
Lyme arthritis occurs in up to 60% of untreated people, typically starting about six months after infection.[22] It usually affects only one or a few joints, often a knee or possibly the hip, other large joints, or the temporomandibular joint.[29][39] There is usually large joint effusion and swelling, but only mild or moderate pain.[29] Without treatment, swelling and pain typically resolve over time but periodically return.[29] Baker’s cysts may form and rupture. In some cases, joint erosion occurs.
Chronic neurologic symptoms occur in up to 5% of untreated people.[40] A peripheral neuropathy or polyneuropathy may develop, causing abnormal sensations such as numbness, tingling or burning starting at the feet or hands and over time possibly moving up the limbs. A test may show reduced sensation of vibrations in the feet. An affected person may feel as if wearing a stocking or glove without actually doing so.[29]
A neurologic syndrome called Lyme encephalopathy is associated with subtle memory and cognitive difficulties, insomnia, a general sense of feeling unwell, and changes in personality.[41] However, problems such as depression and fibromyalgia are as common in people with Lyme disease as in the general population.[42][43]
Lyme can cause a chronic encephalomyelitis that resembles multiple sclerosis. It may be progressive and can involve cognitive impairment, brain fog, migraines, balance issues, weakness in the legs, awkward gait, facial palsy, bladder problems, vertigo, and back pain. In rare cases, untreated Lyme disease may cause frank psychosis, which has been misdiagnosed as schizophrenia or bipolar disorder. Panic attacks and anxiety can occur; also, delusional behavior may be seen, including somatoform delusions, sometimes accompanied by a depersonalization or derealization syndrome, where the people begin to feel detached from themselves or from reality.[44][45]
Acrodermatitis chronica atrophicans (ACA) is a chronic skin disorder observed primarily in Europe among the elderly.[38] ACA begins as a reddish-blue patch of discolored skin, often on the backs of the hands or feet. The lesion slowly atrophies over several weeks or months, with the skin becoming first thin and wrinkled and then, if untreated, completely dry and hairless.[46]
Cause[edit]
Borrelia bacteria, the causative agent of Lyme disease, magnified
Ixodes scapularis, the primary vector of Lyme disease in eastern North America
Tick Ixodes ricinus, developmental stages
Lyme disease is caused by spirochetes, spiral bacteria from the genus Borrelia. Spirochetes are surrounded by peptidoglycan and flagella, along with an outer membrane similar to Gram-negative bacteria. Because of their double-membrane envelope, Borrelia bacteria are often mistakenly described as Gram negative despite the considerable differences in their envelope components from Gram-negative bacteria.[47] The Lyme-related Borrelia species are collectively known as Borrelia burgdorferi sensu lato, and show a great deal of genetic diversity.
B. burgdorferi sensu lato is made up of 21 closely related species, but only four clearly cause Lyme disease: B. mayonii (found in North America), B. burgdorferi sensu stricto (predominant in North America, but also present in Europe), B. afzelii, and B. garinii (both predominant in Eurasia).[48][49][10] Some studies have also proposed that B. bissettii and B. valaisiana may sometimes infect humans, but these species do not seem to be important causes of disease.[50][51]
Transmission[edit]
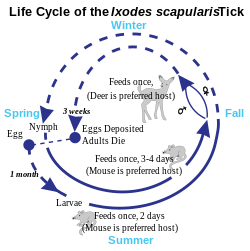
Lyme disease is classified as a zoonosis, as it is transmitted to humans from a natural reservoir among small mammals and birds by ticks that feed on both sets of hosts.[52] Hard-bodied ticks of the genus Ixodes are the main vectors of Lyme disease (also the vector for Babesia).[53] Most infections are caused by ticks in the nymphal stage, because they are very small and thus may feed for long periods of time undetected.[52] Nymphal ticks are generally the size of a poppy seed and sometimes with a dark head and a translucent body.[54] Or, the nymphal ticks can be darker.[55] (The younger larval ticks are very rarely infected.[56]) Although deer are the preferred hosts of adult deer ticks, and tick populations are much lower in the absence of deer, ticks generally do not acquire Borrelia from deer, instead they obtain them from infected small mammals such as the white-footed mouse, and occasionally birds.[57] Areas where Lyme is common are expanding.[58]
Within the tick midgut, the Borrelia‘s outer surface protein A (OspA) binds to the tick receptor for OspA, known as TROSPA. When the tick feeds, the Borrelia downregulates OspA and upregulates OspC, another surface protein. After the bacteria migrate from the midgut to the salivary glands, OspC binds to Salp15, a tick salivary protein that appears to have immunosuppressive effects that enhance infection.[59] Successful infection of the mammalian host depends on bacterial expression of OspC.[60]
Tick bites often go unnoticed because of the small size of the tick in its nymphal stage, as well as tick secretions that prevent the host from feeling any itch or pain from the bite. However, transmission is quite rare, with only about 1.2 to 1.4 percent of recognized tick bites resulting in Lyme disease.[61]
In Europe, the vector is Ixodes ricinus, which is also called the sheep tick or castor bean tick.[62] In China, Ixodes persulcatus (the taiga tick) is probably the most important vector.[63] In North America, the black-legged tick or deer tick (Ixodes scapularis) is the main vector on the East Coast.[56]
The lone star tick (Amblyomma americanum), which is found throughout the Southeastern United States as far west as Texas, is unlikely to transmit the Lyme disease spirochetes,[64] though it may be implicated in a related syndrome called southern tick-associated rash illness, which resembles a mild form of Lyme disease.[65]
On the West Coast of the United States, the main vector is the western black-legged tick (Ixodes pacificus).[66] The tendency of this tick species to feed predominantly on host species such as the Western Fence Lizard that are resistant to Borrelia infection appears to diminish transmission of Lyme disease in the West.[67][68]
Transmission can occur across the placenta during pregnancy and as with a number of other spirochetal diseases, adverse pregnancy outcomes are possible with untreated infection; prompt treatment with antibiotics reduces or eliminates this risk.[69][70][71][72][73]
While Lyme spirochetes have been found in insects, as well as ticks,[74] reports of actual infectious transmission appear to be rare.[75] Lyme spirochete DNA has been found in semen[76] and breast milk.[77] However, according to the CDC, live spirochetes have not been found in breast milk, urine, or semen and thus is not sexually transmitted.[78]
Tick-borne coinfections[edit]
Ticks that transmit B. burgdorferi to humans can also carry and transmit several other parasites, such as Theileria microti and Anaplasma phagocytophilum, which cause the diseases babesiosis and human granulocytic anaplasmosis (HGA), respectively.[79] Among people with early Lyme disease, depending on their location, 2–12% will also have HGA and 2–40% will have babesiosis.[80] Ticks in certain regions, including the lands along the eastern Baltic Sea, also transmit tick-borne encephalitis.[81]
Coinfections complicate Lyme symptoms, especially diagnosis and treatment. It is possible for a tick to carry and transmit one of the coinfections and not Borrelia, making diagnosis difficult and often elusive. The Centers for Disease Control and Prevention studied 100 ticks in rural New Jersey, and found 55% of the ticks were infected with at least one of the pathogens.[82]
Pathophysiology[edit]
B. burgdorferi can spread throughout the body during the course of the disease, and has been found in the skin, heart, joints, peripheral nervous system, and central nervous system.[60][83] Many of the signs and symptoms of Lyme disease are a consequence of the immune response to spirochete in those tissues.[40]
B. burgdorferi is injected into the skin by the bite of an infected Ixodes tick. Tick saliva, which accompanies the spirochete into the skin during the feeding process, contains substances that disrupt the immune response at the site of the bite.[84] This provides a protective environment where the spirochete can establish infection. The spirochetes multiply and migrate outward within the dermis. The host inflammatory response to the bacteria in the skin causes the characteristic circular EM lesion.[60] Neutrophils, however, which are necessary to eliminate the spirochetes from the skin, fail to appear in necessary numbers in the developing EM lesion because tick saliva inhibits neutrophil function. This allows the bacteria to survive and eventually spread throughout the body.[85]
Days to weeks following the tick bite, the spirochetes spread via the bloodstream to joints, heart, nervous system, and distant skin sites, where their presence gives rise to the variety of symptoms of the disseminated disease. The spread of B. burgdorferi is aided by the attachment of the host protease plasmin to the surface of the spirochete.[86]
If untreated, the bacteria may persist in the body for months or even years, despite the production of B. burgdorferi antibodies by the immune system.[87] The spirochetes may avoid the immune response by decreasing expression of surface proteins that are targeted by antibodies, antigenic variation of the VlsE surface protein, inactivating key immune components such as complement, and hiding in the extracellular matrix, which may interfere with the function of immune factors.[88][89]
In the brain, B. burgdorferi may induce astrocytes to undergo astrogliosis (proliferation followed by apoptosis), which may contribute to neurodysfunction.[90] The spirochetes may also induce host cells to secrete quinolinic acid, which stimulates the NMDA receptor on nerve cells, which may account for the fatigue and malaise observed with Lyme encephalopathy.[91] In addition, diffuse white matter pathology during Lyme encephalopathy may disrupt gray matter connections, and could account for deficits in attention, memory, visuospatial ability, complex cognition, and emotional status. White matter disease may have a greater potential for recovery than gray matter disease, perhaps because the neuronal loss is less common. Resolution of MRI white matter hyperintensities after antibiotic treatment has been observed.[92]
Tryptophan, a precursor to serotonin, appears to be reduced within the central nervous system in a number of infectious diseases that affect the brain, including Lyme.[93] Researchers are investigating if this neurohormone secretion is the cause of neuropsychiatric disorders developing in some people with borreliosis.[94]
Immunological studies[edit]
Exposure to the Borrelia bacterium during Lyme disease possibly causes a long-lived and damaging inflammatory response,[95] a form of pathogen-induced autoimmune disease.[96] The production of this reaction might be due to a form of molecular mimicry, where Borrelia avoids being killed by the immune system by resembling normal parts of the body’s tissues.[97][98]
Chronic symptoms from an autoimmune reaction could explain why some symptoms persist even after the spirochetes have been eliminated from the body. This hypothesis may explain why chronic arthritis persists after antibiotic therapy, similar to rheumatic fever, but its wider application is controversial.[99][100]
Diagnosis[edit]
Lyme disease is diagnosed based on symptoms, objective physical findings (such as erythema migrans (EM) rash, facial palsy, or arthritis), history of possible exposure to infected ticks, and possibly laboratory tests.[2][22] People with symptoms of early Lyme disease should have a total body skin examination for EM rashes and asked whether EM-type rashes had manifested within the last 1–2 months.[29] Presence of an EM rash and recent tick exposure (i.e., being outdoors in a likely tick habitat where Lyme is common, within 30 days of the appearance of the rash) are sufficient for Lyme diagnosis; no laboratory confirmation is needed or recommended.[2][22][101][102] Most people who get infected do not remember a tick or a bite, and the EM rash need not look like a bull’s eye (most EM rashes in the U.S. do not) or be accompanied by any other symptoms.[2][103] In the U.S., Lyme is most common in the New England and Mid-Atlantic states and parts of Wisconsin and Minnesota, but it is expanding into other areas.[58] Several bordering areas of Canada also have high Lyme risk.[104]
In the absence of an EM rash or history of tick exposure, Lyme diagnosis depends on laboratory confirmation.[53][105] The bacteria that cause Lyme disease are difficult to observe directly in body tissues and also difficult and too time-consuming to grow in the laboratory.[2][53] The most widely used tests look instead for presence of antibodies against those bacteria in the blood.[106] A positive antibody test result does not by itself prove active infection, but can confirm an infection that is suspected because of symptoms, objective findings, and history of tick exposure in a person.[53] Because as many as 5–20% of the normal population have antibodies against Lyme, people without history and symptoms suggestive of Lyme disease should not be tested for Lyme antibodies: a positive result would likely be false, possibly causing unnecessary treatment.[29][31]
In some cases, when history, signs, and symptoms are strongly suggestive of early disseminated Lyme disease, empiric treatment may be started and reevaluated as laboratory test results become available.[34][107]
Laboratory testing[edit]
Tests for antibodies in the blood by ELISA and Western blot is the most widely used method for Lyme diagnosis. A two-tiered protocol is recommended by the Centers for Disease Control and Prevention (CDC): the sensitive ELISA test is performed first, and if it is positive or equivocal, then the more specific Western blot is run.[108] The immune system takes some time to produce antibodies in quantity. After Lyme infection onset, antibodies of types IgM and IgG usually can first be detected respectively at 2–4 weeks and 4–6 weeks, and peak at 6–8 weeks.[109] When an EM rash first appears, detectable antibodies may not be present. Therefore, it is recommended that testing not be performed and diagnosis be based on the presence of the EM rash.[29] Up to 30 days after suspected Lyme infection onset, infection can be confirmed by detection of IgM or IgG antibodies; after that, it is recommended that only IgG antibodies be considered.[109] A positive IgM and negative IgG test result after the first month of infection is generally indicative of a false positive result.[110] The number of IgM antibodies usually collapses 4–6 months after infection, while IgG antibodies can remain detectable for years.[109]
Other tests may be used in neuroborreliosis cases. In Europe, neuroborreliosis is usually caused by Borrelia garinii and almost always involves lymphocytic pleocytosis, i.e. the densities of lymphocytes (infection-fighting cells) and protein in the cerebrospinal fluid (CSF) typically rise to characteristically abnormal levels, while glucose level remains normal.[32][29][33] Additionally, the immune system produces antibodies against Lyme inside the intrathecal space, which contains the CSF.[29][33] Demonstration by lumbar puncture and CSF analysis of pleocytosis and intrathecal antibody production are required for definite diagnosis of neuroborreliosis in Europe (except in cases of peripheral neuropathy associated with acrodermatitis chronica atrophicans, which usually is caused by Borrelia afzelii and confirmed by blood antibody tests).[31] In North America, neuroborreliosis is caused by Borrelia burgdorferi and may not be accompanied by the same CSF signs; they confirm a diagnosis of central nervous system (CNS) neuroborreliosis if positive, but do not exclude it if negative.[111] American guidelines consider CSF analysis optional when symptoms appear to be confined to the peripheral nervous system (PNS), e.g. facial palsy without overt meninigitis symptoms.[29][112] Unlike blood and intrathecal antibody tests, CSF pleocytosis tests revert to normal after infection ends and therefore can be used as objective markers of treatment success and inform decisions on whether to retreat.[33] In infection involving the PNS, electromyography and nerve conduction studies can be used to monitor objectively the response to treatment.[32]
In Lyme carditis, electrocardiograms are used to evidence heart conduction abnormalities, while echocardiography may show myocardial dysfunction.[36] Biopsy and confirmation of Borrelia cells in myocardial tissue may be used in specific cases but are usually not done because of risk of the procedure.[36]
Polymerase chain reaction (PCR) tests for Lyme disease have also been developed to detect the genetic material (DNA) of the Lyme disease spirochete. Culture or PCR are the current means for detecting the presence of the organism, as serologic studies only test for antibodies of Borrelia. PCR has the advantage of being much faster than culture. However, PCR tests are susceptible to false positive results, e.g. by detection of debris of dead Borrelia cells or specimen contamination.[113][31] Even when properly performed, PCR often shows false negative results because few Borrelia cells can be found in blood and cerebrospinal fluid (CSF) during infection.[114][31] Hence, PCR tests are recommended only in special cases, e.g. diagnosis of Lyme arthritis, because it is a highly sensitive way of detecting ospA DNA in synovial fluid.[115] Although sensitivity of PCR in CSF is low, its use may be considered when intrathecal antibody production test results are suspected of being falsely negative, e.g. in very early (< 6 weeks) neuroborreliosis or in immunosuppressed people.[31]
Several other forms of laboratory testing for Lyme disease are available, some of which have not been adequately validated. OspA antigens, shed by live Borrelia bacteria into urine, are a promising technique being studied.[116] The use of nanotrap particles for their detection is being looked at and the OspA has been linked to active symptoms of Lyme.[117][118] High titers of either immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies to Borrelia antigens indicate disease, but lower titers can be misleading, because the IgM antibodies may remain after the initial infection, and IgG antibodies may remain for years.[119]
The CDC does not recommend urine antigen tests, PCR tests on urine, immunofluorescent staining for cell-wall-deficient forms of B. burgdorferi, and lymphocyte transformation tests.[114]
Imaging[edit]
Neuroimaging is controversial in whether it provides specific patterns unique to neuroborreliosis, but may aid in differential diagnosis and in understanding the pathophysiology of the disease.[120] Though controversial, some evidence shows certain neuroimaging tests can provide data that are helpful in the diagnosis of a person. Magnetic resonance imaging (MRI) and single-photon emission computed tomography (SPECT) are two of the tests that can identify abnormalities in the brain of a person affected with this disease. Neuroimaging findings in an MRI include lesions in the periventricular white matter, as well as enlarged ventricles and cortical atrophy. The findings are considered somewhat unexceptional because the lesions have been found to be reversible following antibiotic treatment. Images produced using SPECT show numerous areas where an insufficient amount of blood is being delivered to the cortex and subcortical white matter. However, SPECT images are known to be nonspecific because they show a heterogeneous pattern in the imaging. The abnormalities seen in the SPECT images are very similar to those seen in people with cerebral vacuities and Creutzfeldt–Jakob disease, which makes them questionable.[121]
Differential diagnosis[edit]
Community clinics have been reported to misdiagnose 23–28% of Erythema migrans (EM) rashes and 83% of other objective manifestations of early Lyme disease.[105] EM rashes are often misdiagnosed as spider bites, cellulitis, or shingles.[105] Many misdiagnoses are credited to the widespread misconception that EM rashes should look like a bull’s eye.[2] Actually, the key distinguishing features of the EM rash are the speed and extent to which it expands, respectively up to 2–3 cm/day and a diameter of at least 5 cm, and in 50% of cases more than 16 cm. The rash expands away from its center, which may or may not look different or be separated by ring-like clearing from the rest of the rash.[22][23] Compared to EM rashes, spider bites are more common in the limbs, tend to be more painful and itchy or become swollen, and some may cause necrosis (sinking dark blue patch of dead skin).[22][2] Cellulitis most commonly develops around a wound or ulcer, is rarely circular, and is more likely to become swollen and tender.[22][2] EM rashes often appear at sites that are unusual for cellulitis, such as the armpit, groin, abdomen, or back of knee.[22] Like Lyme, shingles often begins with headache, fever, and fatigue, which are followed by pain or numbness. However, unlike Lyme, in shingles these symptoms are usually followed by appearance of rashes composed of multiple small blisters along a nerve’s dermatome, and shingles can also be confirmed by quick laboratory tests.[122]
Facial palsy caused by Lyme disease (LDFP) is often misdiagnosed as Bell’s palsy.[34] Although Bell’s palsy is the most common type of one-sided facial palsy (about 70% of cases), LDFP can account for about 25% of cases of facial palsy in areas where Lyme disease is common.[34] Compared to LDFP, Bell’s palsy much less frequently affects both sides of the face.[34] Even though LDFP and Bell’s palsy have similar symptoms and evolve similarly if untreated, corticosteroid treatment is beneficial for Bell’s Palsy, while being detrimental for LDFP.[34] Recent history of exposure to a likely tick habitat during warmer months, EM rash, viral-like symptoms such as headache and fever, and/or palsy in both sides of the face should be evaluated for likelihood of LDFP; if it is more than minimal, empiric therapy with antibiotics should be initiated, without corticosteroids, and reevaluated upon completion of laboratory tests for Lyme disease.[34]
Unlike viral meningitis, Lyme lymphocytic meningitis tends to not cause fever, last longer, and recur.[32][29] Lymphocytic meningitis is also characterized by possibly co-occurring with EM rash, facial palsy, or partial vision obstruction and having much lower percentage of polymorphonuclear leukocytes in CSF.[29]
Lyme radiculopathy affecting the limbs is often misdiagnosed as a radiculopathy caused by nerve root compression, such as sciatica.[105][123] Although most cases of radiculopathy are compressive and resolve with conservative treatment (e.g., rest) within 4–6 weeks, guidelines for managing radiculopathy recommend first evaluating risks of other possible causes that, although less frequent, require immediate diagnosis and treatment, including infections such as Lyme and shingles.[124] A history of outdoor activities in likely tick habitats in the last 3 months possibly followed by a rash or viral-like symptoms, and current headache, other symptoms of lymphocytic meningitis, or facial palsy would lead to suspicion of Lyme disease and recommendation of serological and lumbar puncture tests for confirmation.[124]
Lyme radiculopathy affecting the trunk can be misdiagnosed as myriad other conditions, such as diverticulitis and acute coronary syndrome.[35][105] Diagnosis of late-stage Lyme disease is often complicated by a multifaceted appearance and nonspecific symptoms, prompting one reviewer to call Lyme the new “great imitator”.[125] Lyme disease may be misdiagnosed as multiple sclerosis, rheumatoid arthritis, fibromyalgia, chronic fatigue syndrome, lupus, Crohn’s disease, HIV, or other autoimmune and neurodegenerative diseases. As all people with later-stage infection will have a positive antibody test, simple blood tests can exclude Lyme disease as a possible cause of a person’s symptoms.[126]
Prevention[edit]
Tick bites may be prevented by avoiding or reducing time in likely tick habitats and taking precautions while in and when getting out of one.[127]
Most Lyme human infections are caused by Ixodes nymph bites between April and September.[22][127] Ticks prefer moist, shaded locations in woodlands, shrubs, tall grasses and leaf litter or wood piles.[22][128] Tick densities tend to be highest in woodlands, followed by unmaintained edges between woods and lawns (about half as high), ornamental plants and perennial groundcover (about a quarter), and lawns (about 30 times less).[129] Ixodes larvae and nymphs tend to be abundant also where mice nest, such as stone walls and wood logs.[129] Ixodes larvae and nymphs typically wait for potential hosts (“quest”) on leaves or grasses close to the ground with forelegs outstretched; when a host brushes against its limbs, the tick rapidly clings and climbs on the host looking for a skin location to bite.[130] In Northeastern United States, 69% of tick bites are estimated to happen in residences, 11% in schools or camps, 9% in parks or recreational areas, 4% at work, 3% while hunting, and 4% in other areas.[129] Activities associated with tick bites around residences include yard work, brush clearing, gardening, playing in the yard, and letting into the house dogs or cats that roam outside in woody or grassy areas.[129][127] In parks, tick bites often happen while hiking or camping.[129] Walking on a mowed lawn or center of a trail without touching adjacent vegetation is less risky than crawling or sitting on a log or stone wall.[129][131] Pets should not be allowed to roam freely in likely tick habitats.[128]
As a precaution, CDC recommends soaking or spraying clothes, shoes, and camping gear such as tents, backpacks and sleeping bags with 0.5% permethrin solution and hanging them to dry before use.[127][132] Permethrin is odorless and safe for humans but highly toxic to ticks.[133] After crawling on permethrin-treated fabric for as few as 10–20 seconds, tick nymphs become irritated and fall off or die.[133][134] Permethrin-treated closed-toed shoes and socks reduce by 74 times the number of bites from nymphs that make first contact with a shoe of a person also wearing treated shorts (because nymphs usually quest near the ground, this is a typical contact scenario).[133] Better protection can be achieved by tucking permethrin-treated trousers (pants) into treated socks and a treated long-sleeve shirt into the trousers so as to minimize gaps through which a tick might reach the wearer’s skin.[131] Light-colored clothing may make it easier to see ticks and remove them before they bite.[131] Military and outdoor workers’ uniforms treated with permethrin have been found to reduce the number of bite cases by 80–95%.[134] Permethrin protection lasts several weeks of wear and washings in customer-treated items and up to 70 washings for factory-treated items.[132] Permethrin should not be used on human skin, underwear or cats.[132][135]
The EPA recommends several tick repellents for use on exposed skin, including DEET, picaridin, IR3535 (a derivative of amino acid beta-alanine), oil of lemon eucalyptus (OLE, a natural compound) and OLE’s active ingredient para-menthane-diol (PMD).[127][136][137] Unlike permethrin, repellents repel but do not kill ticks, protect for only several hours after application, and may be washed off by sweat or water.[132] The most popular repellent is DEET in the U.S. and picaridin in Europe.[137] Unlike DEET, picaridin is odorless and is less likely to irritate the skin or harm fabric or plastics.[137] Repellents with higher concentration may last longer but are not more effective; against ticks, 20% picaridin may work for 8 hours vs. 55–98.11% DEET for 5–6 hours or 30–40% OLE for 6 hours.[132][136] Repellents should not be used under clothes, on eyes, mouth, wounds or cuts, or on babies younger than 2 months (3 years for OLE or PMD).[132][127] If sunscreen is used, repellent should be applied on top of it.[132] Repellents should not be sprayed directly on a face, but should instead be sprayed on a hand and then rubbed on the face.[132]
After coming indoors, clothes, gear and pets should be checked for ticks.[127] Clothes can be put into a hot dryer for 10 minutes to kill ticks (just washing or warm dryer are not enough).[127] Showering as soon as possible, looking for ticks over the entire body, and removing them reduce risk of infection.[127] Unfed tick nymphs are the size of a poppy seed, but a day or two after biting and attaching themselves to a person, they look like a small blood blister.[138] The following areas should be checked especially carefully: armpits, between legs, back of knee, bellybutton, trunk, and in children ears, neck and hair.[127]
Tick removal[edit]
Attached ticks should be removed promptly. Risk of infection increases with time of attachment, but in North America risk of Lyme disease is small if the tick is removed within 36 hours.[139] CDC recommends inserting a fine-tipped tweezer between the skin and the tick, grasping very firmly, and pulling the closed tweezer straight away from the skin without twisting, jerking, squeezing or crushing the tick.[140] After tick removal, any tick parts remaining in the skin should be removed with the tweezer, if possible.[140] Wound and hands should then be cleaned with alcohol or soap and water.[140] The tick may be disposed by placing it in a container with alcohol, sealed bag, tape or flushed down the toilet.[140] The bitten person should write down where and when the bite happened so that this can be informed to a doctor if the person gets a rash or flu-like symptoms in the following several weeks.[140] CDC recommends not using fingers, nail polish, petroleum jelly or heat on the tick to try to remove it.[140]
In Australia, where the Australian paralysis tick is prevalent, the Australasian Society of Clinical Immunology and Allergy recommends not using tweezers to remove ticks, because if the person is allergic, anaphylaxis could result.[141] Instead, a product should be sprayed on the tick to cause it to freeze and then drop off.[141] A doctor would use liquid nitrogen, but products available from chemists for freezing warts can be used instead.[142] Another method originating from Australia consists in using about 20 cm of dental floss or fishing line for slowly tying an overhand knot between the skin and the tick and then pulling it away from the skin.[143][144]
Preventive antibiotics[edit]
The risk of infectious transmission increases with the duration of tick attachment.[22] It requires between 36 and 48 hours of attachment for the bacteria that causes Lyme to travel from within the tick into its saliva.[22] If a deer tick that is sufficiently likely to be carrying Borrelia is found attached to a person and removed, and if the tick has been attached for 36 hours or is engorged, a single dose of doxycycline administered within the 72 hours after removal may reduce the risk of Lyme disease. It is not generally recommended for all people bitten, as development of infection is rare: about 50 bitten people would have to be treated this way to prevent one case of erythema migrans (i.e. the typical rash found in about 70–80% of people infected).[2][22]
Garden landscaping[edit]
Several landscaping practices may reduce risk of tick bites in residential yards.[138][145] The lawn should be kept mowed, leaf litter and weeds removed and groundcover use avoided.[138] Woodlands, shrubs, stone walls and wood piles should be separated from the lawn by a 3-ft-wide rock or woodchip barrier.[145] Without vegetation on the barrier, ticks will tend not to cross it; acaricides may also be sprayed on it to kill ticks.[145] A sun-exposed tick-safe zone at least 9 ft from the barrier should concentrate human activity on the yard, including any patios, playgrounds and gardening.[145] Materials such as wood decking, concrete, bricks, gravel or woodchips may be used on the ground under patios and playgrounds so as to discourage ticks there.[138] An 8-ft-high fence may be added to keep deer away from the tick-safe zone.[145][138]
Occupational exposure[edit]
Outdoor workers are at risk of Lyme disease if they work at sites with infected ticks. This includes construction, landscaping, forestry, brush clearing, land surveying, farming, railroad work, oil field work, utility line work, park or wildlife management.[146][147] U.S. workers in the northeastern and north-central states are at highest risk of exposure to infected ticks. Ticks may also transmit other tick-borne diseases to workers in these and other regions of the country. Worksites with woods, bushes, high grass or leaf litter are likely to have more ticks. Outdoor workers should be most careful to protect themselves in the late spring and summer when young ticks are most active.[148]
Host animals[edit]
Lyme and other deer tick-borne diseases can sometimes be reduced by greatly reducing the deer population on which the adult ticks depend for feeding and reproduction. Lyme disease cases fell following deer eradication on an island, Monhegan, Maine,[149] and following deer control in Mumford Cove, Connecticut.[150] It is worth noting that eliminating deer may lead to a temporary increase in tick density.[151]
For example, in the U.S., reducing the deer population to levels of 8 to 10 per square mile (from the current levels of 60 or more deer per square mile in the areas of the country with the highest Lyme disease rates) may reduce tick numbers and reduce the spread of Lyme and other tick-borne diseases.[152] However, such a drastic reduction may be very difficult to implement in many areas, and low to moderate densities of deer or other large mammal hosts may continue to feed sufficient adult ticks to maintain larval densities at high levels. Routine veterinary control of ticks of domestic animals, including livestock, by use of acaricides can contribute to reducing exposure of humans to ticks.
In Europe, known reservoirs of Borrelia burgdorferi were 9 small mammals, 7 medium-sized mammals and 16 species of birds (including passerines, sea-birds and pheasants).[153] These animals seem to transmit spirochetes to ticks and thus participate in the natural circulation of B. burgdorferi in Europe. The house mouse is also suspected as well as other species of small rodents, particularly in Eastern Europe and Russia.[153] “The reservoir species that contain the most pathogens are the European roe deer Capreolus capreolus;[154] “it does not appear to serve as a major reservoir of B. burgdorferi” thought Jaenson & al. (1992)[155] (incompetent host for B. burgdorferi and TBE virus) but it is important for feeding the ticks,[156] as red deer and wild boars (Sus scrofa),[157] in which one Rickettsia and three Borrelia species were identified”,[154] with high risks of coinfection in roe deer.[158] Nevertheless, in the 2000s, in roe deer in Europe “two species of Rickettsia and two species of Borrelia were identified“.[157]
Vaccination[edit]
A recombinant vaccine against Lyme disease, based on the outer surface protein A (ospA) of B. burgdorferi, was developed by SmithKline Beecham. In clinical trials involving more than 10,000 people, the vaccine, called LYMErix, was found to confer protective immunity to Borrelia in 76% of adults and 100% of children with only mild or moderate and transient adverse effects.[159] LYMErix was approved on the basis of these trials by the Food and Drug Administration (FDA) on 21 December 1998.
Following approval of the vaccine, its entry in clinical practice was slow for a variety of reasons, including its cost, which was often not reimbursed by insurance companies.[160] Subsequently, hundreds of vaccine recipients reported they had developed autoimmune and other side effects. Supported by some advocacy groups, a number of class-action lawsuits were filed against GlaxoSmithKline, alleging the vaccine had caused these health problems. These claims were investigated by the FDA and the Centers for Disease Control, which found no connection between the vaccine and the autoimmune complaints.[161]
Despite the lack of evidence that the complaints were caused by the vaccine, sales plummeted and LYMErix was withdrawn from the U.S. market by GlaxoSmithKline in February 2002,[162] in the setting of negative media coverage and fears of vaccine side effects.[161][163] The fate of LYMErix was described in the medical literature as a “cautionary tale”;[163] an editorial in Nature cited the withdrawal of LYMErix as an instance in which “unfounded public fears place pressures on vaccine developers that go beyond reasonable safety considerations.”[20] The original developer of the OspA vaccine at the Max Planck Institute told Nature: “This just shows how irrational the world can be … There was no scientific justification for the first OspA vaccine LYMErix being pulled.”[161]
Vaccines have been formulated and approved for prevention of Lyme disease in dogs. Currently, three Lyme disease vaccines are available. LymeVax, formulated by Fort Dodge Laboratories, contains intact dead spirochetes which expose the host to the organism. Galaxy Lyme, Intervet-Schering-Plough‘s vaccine, targets proteins OspC and OspA. The OspC antibodies kill any of the bacteria that have not been killed by the OspA antibodies. Canine Recombinant Lyme, formulated by Merial, generates antibodies against the OspA protein so a tick feeding on a vaccinated dog draws in blood full of anti-OspA antibodies, which kill the spirochetes in the tick’s gut before they are transmitted to the dog.[164]
A hexavalent (OspA) protein subunit-based vaccine candidate VLA15 was granted fast track designation by the U.S. Food and Drug Administration in 2017 which will allow further study.[165]
Treatment[edit]
Antibiotics are the primary treatment.[2][22] The specific approach to their use is dependent on the individual affected and the stage of the disease.[22] For most people with early localized infection, oral administration of doxycycline is widely recommended as the first choice, as it is effective against not only Borrelia bacteria but also a variety of other illnesses carried by ticks.[22] People taking doxycycline should avoid sun exposure because of higher risk of sunburns.[29] Doxycycline is contraindicated in children younger than eight years of age and women who are pregnant or breastfeeding;[22] alternatives to doxycycline are amoxicillin, cefuroxime axetil, and azithromycin.[22] Azithromicyn is recommended only in case of intolerance to the other antibiotics.[29] The standard treatment for cellulitis, cephalexin, is not useful for Lyme disease.[29] When it is unclear if a rash is caused by Lyme or cellulitis, the IDSA recommends treatment with cefuroxime or amoxicillin/clavulanic acid, as these are effective against both infections.[29] Individuals with early disseminated or late Lyme infection may have symptomatic cardiac disease, Lyme arthritis, or neurologic symptoms like facial palsy, radiculopathy, meningitis, or peripheral neuropathy.[22] Intravenous administration of ceftriaxone is recommended as the first choice in these cases;[22] cefotaxime and doxycycline are available as alternatives.[22]
These treatment regimens last from one to four weeks.[22] Neurologic complications of Lyme disease may be treated with doxycycline as it can be taken by mouth and has a lower cost, although in North America evidence of efficacy is only indirect.[112] In case of failure, guidelines recommend retreatment with injectable ceftriaxone.[112] Several months after treatment for Lyme arthritis, if joint swelling persists or returns, a second round of antibiotics may be considered; intravenous antibiotics are preferred for retreatment in case of poor response to oral antibiotics.[22][29] Outside of that, a prolonged antibiotic regimen lasting more than 28 days is not recommended as no evidence shows it to be effective.[22][166] IgM and IgG antibody levels may be elevated for years even after successful treatment with antibiotics.[22] As antibody levels are not indicative of treatment success, testing for them is not recommended.[22]
Facial palsy may resolve without treatment; however, antibiotic treatment is recommended to stop other Lyme complications.[29] Corticosteroids are not recommended when facial palsy is caused by Lyme disease.[34] In those with facial palsy, frequent use of artificial tears while awake is recommended, along with ointment and a patch or taping the eye closed when sleeping.[34][167]
About a third of people with Lyme carditis need a temporary pacemaker until their heart conduction abnormality resolves, and 21% need to be hospitalized.[36] Lyme carditis should not be treated with corticosteroids.[36]
People with Lyme arthritis should limit their level of physical activity to avoid damaging affected joints, and in case of limping should use crutches.[168] Pain associated with Lyme disease may be treated with nonsteroidal anti-inflammatory drugs (NSAIDs).[29] Corticosteroid joint injections are not recommended for Lyme arthritis that is being treated with antibiotics.[29][168] People with Lyme arthritis treated with intravenous antibiotics or two months of oral antibiotics who continue to have joint swelling two months after treatment and have negative PCR test for Borrelia DNA in the synovial fluid are said to have antibiotic-refractory Lyme arthritis; this is more common after infection by certain Borrelia strains in people with certain genetic and immunologic characteristics.[29][168] Antibiotic-refractory Lyme arthritis may be symptomatically treated with NSAIDs, disease-modifying antirheumatic drugs (DMARDs), or arthroscopic synovectomy.[29] Physical therapy is recommended for adults after resolution of Lyme arthritis.[168]
People receiving treatment should be advised that reinfection is possible and how to prevent it.[107]
Prognosis[edit]
Lyme disease’s typical first sign, the erythema migrans (EM) rash, resolves within several weeks even without treatment.[2] However, in untreated people, the infection often disseminates to the nervous system, heart, or joints, possibly causing permanent damage to body tissues.[29]
People who receive recommended antibiotic treatment within several days of appearance of an initial EM rash have the best prospects.[105] Recovery may not be total or immediate. The percentage of people achieving full recovery in the United States increases from about 64–71% at end of treatment for EM rash to about 84–90% after 30 months; higher percentages are reported in Europe.[169][170] Treatment failure, i.e. persistence of original or appearance of new signs of the disease, occurs only in a few people.[169] Remaining people are considered cured but continue to experience subjective symptoms, e.g. joint or muscle pains or fatigue.[171] These symptoms usually are mild and nondisabling.[171]
People treated only after nervous system manifestations of the disease may end up with objective neurological deficits, in addition to subjective symptoms.[29] In Europe, an average of 32–33 months after initial Lyme symptoms in people treated mostly with doxycycline 200 mg for 14–21 days, the percentage of people with lingering symptoms was much higher among those diagnosed with neuroborreliosis (50%) than among those with only an EM rash (16%).[172] In another European study, 5 years after treatment for neuroborreliosis, lingering symptoms were less common among children (15%) than adults (30%), and in the latter was less common among those treated within 30 days of the first symptom (16%) than among those treated later (39%); among those with lingering symptoms, 54% had daily activities restricted and 19% were on sick leave or incapacitated.[173]
Some data suggest that about 90% of Lyme facial palsies treated with antibiotics recover fully a median of 24 days after appearing and most of the rest recover with only mild abnormality.[174][175] However, in Europe 41% of people treated for facial palsy had other lingering symptoms at followup up to 6 months later, including 28% with numbness or altered sensation and 14% with fatigue or concentration problems.[175] Palsies in both sides of the face are associated with worse and longer time to recovery.[174][175] Historical data suggests that untreated people with facial palsies recover at nearly the same rate, but 88% subsequently have Lyme arthritis.[174][176] Other research shows that synkinesis (involuntary movement of a facial muscle when another one is voluntarily moved) can become evident only 6–12 months after facial palsy appears to be resolved, as damaged nerves regrow and sometimes connect to incorrect muscles.[177] Synkinesis is associated with corticosteroid use.[177] In longer-term follow-up, 16–23% of Lyme facial palsies do not fully recover.[177]
In Europe, about a quarter of people with Bannwarth syndrome (Lyme radiculopathy and lymphocytic meningitis) treated with intravenous ceftriaxone for 14 days an average of 30 days after first symptoms had to be retreated 3–6 months later because of unsatisfactory clinical response or continued objective markers of infection in cerebrospinal fluid; after 12 months, 64% recovered fully, 31% had nondisabling mild or infrequent symptoms that did not require regular use of analgesics, and 5% had symptoms that were disabling or required substantial use of analgesics.[33] The most common lingering nondisabling symptoms were headache, fatigue, altered sensation, joint pains, memory disturbances, malaise, radicular pain, sleep disturbances, muscle pains, and concentration disturbances. Lingering disabling symptoms included facial palsy and other impaired movement.[33]
Recovery from late neuroborreliosis tends to take longer and be less complete than from early neuroborreliosis, probably because of irreversible neurologic damage.[29]
About half the people with Lyme carditis progress to complete heart block, but it usually resolves in a week.[36] Other Lyme heart conduction abnormalities resolve typically within 6 weeks.[36] About 94% of people have full recovery, but 5% need a permanent pacemaker and 1% end up with persistent heart block (the actual percentage may be higher because of unrecognized cases).[36] Lyme myocardial complications usually are mild and self-limiting.[36] However, in some cases Lyme carditis can be fatal.[36]
Recommended antibiotic treatments are effective in about 90% of Lyme arthritis cases, although it can take several months for inflammation to resolve and a second round of antibiotics is often necessary.[29] Antibiotic-refractory Lyme arthritis also eventually resolves, typically within 9–14 months (range 4 months – 4 years); DMARDs or synovectomy can accelerate recovery.[168]
Reinfection is not uncommon. In a U.S. study, 6–11% of people treated for an EM rash had another EM rash within 30 months.[169] The second rash typically is due to infection by a different Borrelia strain.[178]
People who have nonspecific, subjective symptoms such as fatigue, joint and muscle aches, or cognitive difficulties for more than six months after recommended treatment for Lyme disease are said to have post-treatment Lyme disease syndrome. As of 2016 the reason for the lingering symptoms was not known; the condition is generally managed similarly to fibromyalgia or chronic fatigue syndrome.[179]
Epidemiology[edit]
Lyme disease occurs regularly in Northern Hemisphere temperate regions.[180]
Africa[edit]
In northern Africa, B. burgdorferi sensu lato has been identified in Morocco, Algeria, Egypt and Tunisia.[181][182][183]
Lyme disease in sub-Saharan Africa is presently unknown, but evidence indicates it may occur in humans in this region. The abundance of hosts and tick vectors would favor the establishment of Lyme infection in Africa.[184] In East Africa, two cases of Lyme disease have been reported in Kenya.[185]
Asia[edit]
B. burgdorferi sensu lato-infested ticks are being found more frequently in Japan, as well as in northwest China, Nepal, Thailand and far eastern Russia.[186][187] Borrelia has also been isolated in Mongolia.[188]
Europe[edit]
In Europe, Lyme disease is caused by infection with one or more pathogenic European genospecies of the spirochaete B. burgdorferi sensu lato, mainly transmitted by the tick Ixodes ricinus.[189] Cases of B. burgdorferi sensu lato-infected ticks are found predominantly in central Europe, particularly in Slovenia and Austria, but have been isolated in almost every country on the continent.[190] Number of cases in southern Europe, such as Italy and Portugal, is much lower.[191]
United Kingdom[edit]
In the United Kingdom the number of laboratory confirmed cases of Lyme disease has been rising steadily since voluntary reporting was introduced in 1986[192] when 68 cases were recorded in the UK and Republic of Ireland combined.[193] In the UK there were 23 confirmed cases in 1988 and 19 in 1990,[194] but 973 in 2009[192] and 953 in 2010.[195] Provisional figures for the first 3 quarters of 2011 show a 26% increase on the same period in 2010.[196]
It is thought, however, that the actual number of cases is significantly higher than suggested by the above figures, with the UK’s Health Protection Agency estimating that there are between 2,000 and 3,000 cases per year,[195] (with an average of around 15% of the infections acquired overseas[192]), while Dr Darrel Ho-Yen, Director of the Scottish Toxoplasma Reference Laboratory and National Lyme Disease Testing Service, believes that the number of confirmed cases should be multiplied by 10 “to take account of wrongly diagnosed cases, tests giving false results, sufferers who weren’t tested, people who are infected but not showing symptoms, failures to notify and infected individuals who don’t consult a doctor.”[197][198]
Despite Lyme disease (Borrelia burgdorferi infection) being a notifiable disease in Scotland[199] since January 1990[200] which should therefore be reported on the basis of clinical suspicion, it is believed that many GPs are unaware of the requirement.[201] Mandatory reporting, limited to laboratory test results only, was introduced throughout the UK in October 2010, under the Health Protection (Notification) Regulations 2010.[192]
Although there is a greater number of cases of Lyme disease in the New Forest, Salisbury Plain, Exmoor, the South Downs, parts of Wiltshire and Berkshire, Thetford Forest[202] and the West coast and islands of Scotland[203] infected ticks are widespread, and can even be found in the parks of London.[194][204] A 1989 report found that 25% of forestry workers in the New Forest were seropositive, as were between 2% and 4–5% of the general local population of the area.[205][206]
Tests on pet dogs, carried out throughout the country in 2009 indicated that around 2.5% of ticks in the UK may be infected, considerably higher than previously thought.[207][208] It is thought that global warming may lead to an increase in tick activity in the future, as well as an increase in the amount of time that people spend in public parks, thus increasing the risk of infection.[209]
North America[edit]
Many studies in North America have examined ecological and environmental correlates of the number of people affected by Lyme disease. A 2005 study using climate suitability modelling of I. scapularis projected that climate change would cause an overall 213% increase in suitable vector habitat by the year 2080, with northward expansions in Canada, increased suitability in the central U.S., and decreased suitable habitat and vector retraction in the southern U.S.[210] A 2008 review of published studies concluded that the presence of forests or forested areas was the only variable that consistently elevated the risk of Lyme disease whereas other environmental variables showed little or no concordance between studies.[211] The authors argued that the factors influencing tick density and human risk between sites are still poorly understood, and that future studies should be conducted over longer time periods, become more standardized across regions, and incorporate existing knowledge of regional Lyme disease ecology.[211]
Canada[edit]
Owing to changing climate, the range of ticks able to carry Lyme disease has expanded from a limited area of Ontario to include areas of southern Quebec, Manitoba, northern Ontario, southern New Brunswick, southwest Nova Scotia and limited parts of Saskatchewan and Alberta, as well as British Columbia. Cases have been reported as far east as the island of Newfoundland.[104][212][213][214] A model-based prediction by Leighton et al. (2012) suggests that the range of the I. scapularis tick will expand into Canada by 46 km/year over the next decade, with warming climatic temperatures as the main driver of increased speed of spread.[215]
Mexico[edit]
A 2007 study suggests Borrelia burgdorferi infections are endemic to Mexico, from four cases reported between 1999 and 2000.[216]
United States[edit]
CDC map showing the risk of Lyme disease in the United States, particularly its concentration in the Northeast Megalopolis and western Wisconsin.
Each year, approximately 30,000 new cases are reported to the CDC however, this number is likely underestimated. The CDC is currently conducting research on evaluation and diagnostics of the disease and preliminary results suggest the number of new cases to be around 300,000.[217][218]
Lyme disease is the most common tick-borne disease in North America and Europe, and one of the fastest-growing infectious diseases in the United States. Of cases reported to the United States CDC, the ratio of Lyme disease infection is 7.9 cases for every 100,000 persons. In the ten states where Lyme disease is most common, the average was 31.6 cases for every 100,000 persons for the year 2005.[219][220][221]
Although Lyme disease has been reported in all states[217][222] about 99% of all reported cases are confined to just five geographic areas (New England, Mid-Atlantic, East-North Central, South Atlantic, and West North-Central).[223] New 2011 CDC Lyme case definition guidelines are used to determine confirmed CDC surveillance cases.[224]
Effective January 2008, the CDC gives equal weight to laboratory evidence from 1) a positive culture for B. burgdorferi; 2) two-tier testing (ELISA screening and Western blot confirming); or 3) single-tier IgG (old infection) Western blot.[225] Previously, the CDC only included laboratory evidence based on (1) and (2) in their surveillance case definition. The case definition now includes the use of Western blot without prior ELISA screen.[225]
The number of reported cases of the disease has been increasing, as are endemic regions in North America. For example, B. burgdorferi sensu lato was previously thought to be hindered in its ability to be maintained in an enzootic cycle in California, because it was assumed the large lizard population would dilute the number of people affected by B. burgdorferi in local tick populations; this has since been brought into question, as some evidence has suggested lizards can become infected.[226]
Except for one study in Europe,[227] much of the data implicating lizards is based on DNA detection of the spirochete and has not demonstrated that lizards are able to infect ticks feeding upon them.[226][228][229][230] As some experiments suggest lizards are refractory to infection with Borrelia, it appears likely their involvement in the enzootic cycle is more complex and species-specific.[68]
While B. burgdorferi is most associated with ticks hosted by white-tailed deer and white-footed mice, Borrelia afzelii is most frequently detected in rodent-feeding vector ticks, and Borrelia garinii and Borrelia valaisiana appear to be associated with birds. Both rodents and birds are competent reservoir hosts for B. burgdorferi sensu stricto. The resistance of a genospecies of Lyme disease spirochetes to the bacteriolytic activities of the alternative complement pathway of various host species may determine its reservoir host association.[citation needed]
Several similar but apparently distinct conditions may exist, caused by various species or subspecies of Borrelia in North America. A regionally restricted condition that may be related to Borrelia infection is southern tick-associated rash illness (STARI), also known as Masters disease. Amblyomma americanum, known commonly as the lone-star tick, is recognized as the primary vector for STARI. In some parts of the geographical distribution of STARI, Lyme disease is quite rare (e.g., Arkansas), so people in these regions experiencing Lyme-like symptoms—especially if they follow a bite from a lone-star tick—should consider STARI as a possibility. It is generally a milder condition than Lyme and typically responds well to antibiotic treatment.[231]
In recent years there have been 5 to 10 cases a year of a disease similar to Lyme occurring in Montana. It occurs primarily in pockets along the Yellowstone River in central Montana. People have developed a red bull’s-eye rash around a tick bite followed by weeks of fatigue and a fever.[222]
Lyme disease effects are comparable among males and females. A wide range of age groups is affected, though the number of cases is highest among 10- to 19-year-olds. For unknown reasons, Lyme disease is seven times more common among Asians.[232]
South America[edit]
In South America, tick-borne disease recognition and occurrence is rising. In Brazil, a Lyme-like disease known as Baggio–Yoshinari syndrome was identified, caused by microorganisms that do not belong to the B. burgdorferi sensu lato complex and transmitted by ticks of the Amblyomma and Rhipicephalus genera.[233] The first reported case of BYS in Brazil was made in 1992 in Cotia, São Paulo.[234] B. burgdorferi sensu stricto antigens in people have been identified in Colombia,[235] and Bolivia.[citation needed]
History[edit]
The evolutionary history of Borrelia burgdorferi genetics has been the subject of recent studies. One study has found that prior to the reforestation that accompanied post-colonial farm abandonment in New England and the wholesale migration into the mid-west that occurred during the early 19th century, Lyme disease was present for thousands of years in America and had spread along with its tick hosts from the Northeast to the Midwest.[236]
John Josselyn, who visited New England in 1638 and again from 1663 to 1670, wrote “there be infinite numbers of ticks hanging upon the bushes in summer time that will cleave to man’s garments and creep into his breeches, eating themselves in a short time into the very flesh of a man. I have seen the stockings of those that have gone through the woods covered with them.”[237]
This is also confirmed by the writings of Peter Kalm, a Swedish botanist who was sent to America by Linnaeus, and who found the forests of New York “abound” with ticks when he visited in 1749. When Kalm’s journey was retraced 100 years later, the forests were gone and the Lyme bacterium had probably become isolated to a few pockets along the northeast coast, Wisconsin, and Minnesota.[238]
Perhaps the first detailed description of what is now known as Lyme disease appeared in the writings of John Walker after a visit to the island of Jura (Deer Island) off the west coast of Scotland in 1764.[239] He gives a good description both of the symptoms of Lyme disease (with “exquisite pain [in] the interior parts of the limbs”) and of the tick vector itself, which he describes as a “worm” with a body which is “of a reddish color and of a compressed shape with a row of feet on each side” that “penetrates the skin”. Many people from this area of Great Britain emigrated to North America between 1717 and the end of the 18th century.
The examination of preserved museum specimens has found Borrelia DNA in an infected Ixodes ricinus tick from Germany that dates back to 1884, and from an infected mouse from Cape Cod that died in 1894.[238] The 2010 autopsy of Ötzi the Iceman, a 5,300-year-old mummy, revealed the presence of the DNA sequence of Borrelia burgdorferi making him the earliest known human with Lyme disease.[240]
The early European studies of what is now known as Lyme disease described its skin manifestations. The first study dates to 1883 in Breslau, Germany (now Wrocław, Poland), where physician Alfred Buchwald described a man who had suffered for 16 years with a degenerative skin disorder now known as acrodermatitis chronica atrophicans.[241]
At a 1909 research conference, Swedish dermatologist Arvid Afzelius presented a study about an expanding, ring-like lesion he had observed in an older woman following the bite of a sheep tick. He named the lesion erythema migrans.[241] The skin condition now known as borrelial lymphocytoma was first described in 1911.[242]
The modern history of medical understanding of the disease, including its cause, diagnosis, and treatment, has been difficult.[243]
Neurological problems following tick bites were recognized starting in the 1920s. French physicians Garin and Bujadoux described a farmer with a painful sensory radiculitis accompanied by mild meningitis following a tick bite. A large, ring-shaped rash was also noted, although the doctors did not relate it to the meningoradiculitis. In 1930, the Swedish dermatologist Sven Hellerström was the first to propose EM and neurological symptoms following a tick bite were related.[244] In the 1940s, German neurologist Alfred Bannwarth described several cases of chronic lymphocytic meningitis and polyradiculoneuritis, some of which were accompanied by erythematous skin lesions.
Carl Lennhoff, who worked at the Karolinska Institute in Sweden, believed many skin conditions were caused by spirochetes. In 1948, he used a special stain to microscopically observe what he believed were spirochetes in various types of skin lesions, including EM.[245] Although his conclusions were later shown to be erroneous, interest in the study of spirochetes was sparked. In 1949, Nils Thyresson, who also worked at the Karolinska Institute, was the first to treat ACA with penicillin.[246] In the 1950s, the relationship among tick bite, lymphocytoma, EM and Bannwarth’s syndrome was recognized throughout Europe leading to the widespread use of penicillin for treatment in Europe.[247][248]
In 1970, a dermatologist in Wisconsin named Rudolph Scrimenti recognized an EM lesion in a person after recalling a paper by Hellerström that had been reprinted in an American science journal in 1950. This was the first documented case of EM in the United States. Based on the European literature, he treated the person with penicillin.[249]
The full syndrome now known as Lyme disease was not recognized until a cluster of cases originally thought to be juvenile rheumatoid arthritis was identified in three towns in southeastern Connecticut in 1975, including the towns Lyme and Old Lyme, which gave the disease its popular name.[250] This was investigated by physicians David Snydman and Allen Steere of the Epidemic Intelligence Service, and by others from Yale University, including Stephen Malawista, who is credited as a co-discover of the disease.[251] The recognition that the people in the United States had EM led to the recognition that “Lyme arthritis” was one manifestation of the same tick-borne condition known in Europe.[252]
Before 1976, the elements of B. burgdorferi sensu lato infection were called or known as tick-borne meningopolyneuritis, Garin-Bujadoux syndrome, Bannwarth syndrome, Afzelius’s disease,[253] Montauk Knee or sheep tick fever. Since 1976 the disease is most often referred to as Lyme disease,[254][255] Lyme borreliosis or simply borreliosis.[256][257]
In 1980, Steere, et al., began to test antibiotic regimens in adults with Lyme disease.[258] In the same year, New York State Health Dept. epidemiologist Jorge Benach provided Willy Burgdorfer, a researcher at the Rocky Mountain Biological Laboratory, with collections of I. dammini [scapularis] from Shelter Island, New York, a known Lyme-endemic area as part of an ongoing investigation of Rocky Mountain spotted fever. In examining the ticks for rickettsiae, Burgdorfer noticed “poorly stained, rather long, irregularly coiled spirochetes.” Further examination revealed spirochetes in 60% of the ticks. Burgdorfer credited his familiarity with the European literature for his realization that the spirochetes might be the “long-sought cause of ECM and Lyme disease.” Benach supplied him with more ticks from Shelter Island and sera from people diagnosed with Lyme disease. University of Texas Health Science Center researcher Alan Barbour “offered his expertise to culture and immunochemically characterize the organism.” Burgdorfer subsequently confirmed his discovery by isolating, from people with Lyme disease, spirochetes identical to those found in ticks.[259] In June 1982, he published his findings in Science, and the spirochete was named Borrelia burgdorferi in his honor.[260]
After the identification of B. burgdorferi as the causative agent of Lyme disease, antibiotics were selected for testing, guided by in vitro antibiotic sensitivities, including tetracycline antibiotics, amoxicillin, cefuroxime axetil, intravenous and intramuscular penicillin and intravenous ceftriaxone.[261][262] The mechanism of tick transmission was also the subject of much discussion. B. burgdorferi spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.[263]
Society and culture[edit]
Urbanization and other anthropogenic factors can be implicated in the spread of Lyme disease to humans. In many areas, expansion of suburban neighborhoods has led to gradual deforestation of surrounding wooded areas and increased border contact between humans and tick-dense areas. Human expansion has also resulted in a reduction of predators that hunt deer as well as mice, chipmunks and other small rodents—the primary reservoirs for Lyme disease. As a consequence of increased human contact with host and vector, the likelihood of transmission of the disease has greatly increased.[264][265] Researchers are investigating possible links between global warming and the spread of vector-borne diseases, including Lyme disease.[266]
Controversy[edit]
The term “chronic Lyme disease” is controversial and not recognized in the medical literature,[267] and most medical authorities advise against long-term antibiotic treatment for Lyme disease.[29][112][268] Studies have shown that most people diagnosed with “chronic Lyme disease” either have no objective evidence of previous or current infection with B. burgdorferi or are people who should be classified as having post-treatment Lyme disease syndrome (PTLDS), which is defined as continuing or relapsing non-specific symptoms (such as fatigue, musculoskeletal pain, and cognitive complaints) in a person previously treated for Lyme disease.[269]
Pop culture[edit]
The 2008 documentary Under Our Skin courted controversy for promoting ‘chronic Lyme disease.’[270]
American indie rock band Typhoon are noted for having multiple songs which reference or are directly about Lyme disease.[271] The band is led by singer-songwriter Kyle Morton who suffered serious complications from the disease through much of his young adulthood.[272]
Other animals[edit]
Prevention of Lyme disease is an important step in keeping dogs safe in endemic areas. Prevention education and a number of preventive measures are available. First, for dog owners who live near or who often frequent tick-infested areas, routine vaccinations of their dogs is an important step.[273]
Another crucial preventive measure is the use of persistent acaricides, such as topical repellents or pesticides that contain triazapentadienes (Amitraz), phenylpyrazoles (Fipronil), or permethrin (pyrethroids).[274] These acaricides target primarily the adult stages of Lyme-carrying ticks and reduce the number of reproductively active ticks in the environment.[273] Formulations of these ingredients are available in a variety of topical forms, including spot-ons, sprays, powders, impregnated collars, solutions, and shampoos.[274]
Examination of a dog for ticks after being in a tick-infested area is an important precautionary measure to take in the prevention of Lyme disease. Key spots to examine include the head, neck, and ears.[275]
In dogs, a serious long-term prognosis may result in glomerular disease,[276] which is a category of kidney damage that may cause chronic kidney disease.[164] Dogs may also experience chronic joint disease if the disease is left untreated. However, the majority of cases of Lyme disease in dogs result in a complete recovery with, and sometimes without, treatment with antibiotics.[277][verification needed] In rare cases, Lyme disease can be fatal to both humans and dogs.[278]
Lyme disease can also infect deer. The winter tick which has affected moose populations in the 21st century is not a carrier of Lyme.[279]
Research[edit]
In the US, the National Institutes of Health has supported research into bacterial persistence.[280]
References[edit]
- ^ Jump up to:a b c d e f g h i j k “Signs and Symptoms of Lyme Disease”. cdc.gov. 11 January 2013. Archived from the original on 16 January 2013. Retrieved 2 March 2015.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah Shapiro ED (May 2014). “Clinical practice. Lyme disease” (PDF). The New England Journal of Medicine. 370 (18): 1724–1731. doi:10.1056/NEJMcp1314325. PMC 4487875. PMID 24785207. Archived from the original (PDF) on 21 August 2016. Retrieved 5 July 2016.
- ^ Jump up to:a b “Lyme Disease Diagnosis and Testing”. cdc.gov. 10 January 2013. Archived from the original on 2 March 2015. Retrieved 2 March 2015.
- ^ Jump up to:a b Berger, Stephen (2014). Lyme disease: Global Status 2014 Edition. GIDEON Informatics Inc. p. 7. ISBN 9781498803434. Archived from the original on 8 September 2017.
- ^ Aucott JN (June 2015). “Posttreatment Lyme disease syndrome”. Infectious Disease Clinics of North America. 29 (2): 309–323. doi:10.1016/j.idc.2015.02.012. PMID 25999226.
- ^ Johnson RC (1996). “Borrelia”. In Baron S, et al. (eds.). Baron’s Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 978-0-9631172-1-2. PMID 21413339. Archived from the original on 7 February 2009.
- ^ Jump up to:a b “Lyme disease transmission”. cdc.gov. 11 January 2013. Archivedfrom the original on 3 March 2015. Retrieved 2 March 2015.
- ^ Jump up to:a b Steere, AC; Strle, F; Wormser, GP; Hu, LT; Branda, JA; Hovius, JW; Li, X; Mead, PS (15 December 2016). “Lyme borreliosis”. Nature Reviews. Disease Primers. 2: 16090. doi:10.1038/nrdp.2016.90. PMC 5539539. PMID 27976670.
- ^ “Lyme borreliosis” (PDF). ECDC. Archived (PDF) from the original on 29 September 2018. Retrieved 29 September 2018.
- ^ Jump up to:a b Pritt BS, Mead PS, Johnson DK, Neitzel DF, Respicio-Kingry LB, Davis JP, Schiffman E, Sloan LM, Schriefer ME, Replogle AJ, Paskewitz SM, Ray JA, Bjork J, Steward CR, Deedon A, Lee X, Kingry LC, Miller TK, Feist MA, Theel ES, Patel R, Irish CL, Petersen JM (May 2016). “Identification of a novel pathogenic Borrelia species causing Lyme borreliosis with unusually high spirochaetaemia: a descriptive study”. The Lancet. Infectious Diseases. 16(5): 556–564. doi:10.1016/S1473-3099(15)00464-8. PMC 4975683. PMID 26856777.
- ^ “Two-step Laboratory Testing Process”. cdc.gov. 15 November 2011. Archived from the original on 12 March 2015. Retrieved 2 March 2015.
- ^ “Testing of Ticks”. cdc.gov. 4 June 2013. Archived from the original on 19 February 2015. Retrieved 2 March 2015.
Although some commercial groups offer testing, in general this is not recommended
- ^ “Tick Removal”. cdc.gov. 23 June 2014. Archived from the original on 10 March 2015. Retrieved 2 March 2015.
- ^ Jump up to:a b c “Post-Treatment Lyme Disease Syndrome”. cdc.gov. 1 December 2017. Archived from the original on 27 February 2015. Retrieved 20 June2018.
- ^ Regional Disease Vector Ecology Profile: Central Europe. DIANE Publishing. April 2001. p. 136. ISBN 9781428911437. Archived from the original on 8 September 2017.
- ^ Jump up to:a b Williams, Carolyn (2007). Infectious disease epidemiology : theory and practice (2nd ed.). Sudbury, Mass.: Jones and Bartlett Publishers. p. 447. ISBN 9780763728793. Archived from the original on 8 September 2017.
- ^ “Willy Burgdorfer – obituary”. Daily Telegraph. 1 December 2014. Archived from the original on 1 December 2014. Retrieved 1 December2014.
- ^ Baker, PJ (November 2010). “Chronic Lyme disease: in defense of the scientific enterprise”. FASEB Journal. 24 (11): 4175–7. doi:10.1096/fj.10-167247. PMID 20631327. S2CID 36141950.
- ^ Lantos PM (June 2015). “Chronic Lyme disease”. Infectious Disease Clinics of North America. 29 (2): 325–40. doi:10.1016/j.idc.2015.02.006. PMC 4477530. PMID 25999227.
- ^ Jump up to:a b “When a vaccine is safe”. Nature. 439 (7076): 509. February 2006. Bibcode:2006Natur.439Q.509.. doi:10.1038/439509a. PMID 16452935.
- ^ Aronowitz, Robert A (June 2016). “The Rise and Fall of the Lyme Disease Vaccines: A Cautionary Tale for Risk Interventions in American Medicine and Public Health”. The Milbank Quarterly. 90 (2): 250–277. doi:10.1111/j.1468-0009.2012.00663.x. ISSN 0887-378X. PMC 3460208. PMID 22709388.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad Wright WF, Riedel DJ, Talwani R, Gilliam BL (June 2012). “Diagnosis and management of Lyme disease”. American Family Physician. 85 (11): 1086–93. PMID 22962880. Archived from the original on 27 September 2013.
- ^ Jump up to:a b c d Tibbles CD, Edlow JA (20 June 2007). “Does This Patient Have Erithema Migrans?”. JAMA. 297 (23): 2617–27. doi:10.1001/jama.297.23.2617. PMID 17579230.
- ^ Jump up to:a b c “Lyme disease rashes and look-alikes”. Lyme Disease. Centers for Disease Control and Prevention. 21 December 2018. Archived from the original on 2 April 2019. Retrieved 18 April 2019.
- ^ Jump up to:a b c “Lyme disease: erythema migrans”. Lyme disease NICE guideline [NG95]. National Institute for Health and Care Excellence. Archived from the original on 9 May 2019. Retrieved 8 May 2019.
- ^ Jump up to:a b Lyme disease at eMedicine
- ^ Steere AC, Sikand VK, Schoen RT, Nowakowski J (August 2003). “Asymptomatic infection with Borrelia burgdorferi”. Clinical Infectious Diseases. 37 (4): 528–32. doi:10.1086/376914. PMID 12905137. (primary source)
- ^ Jump up to:a b Biesiada G, Czepiel J, Leśniak MR, Garlicki A, Mach T (December 2012). “Lyme disease: review”. Archives of Medical Science. 8 (6): 978–82. doi:10.5114/aoms.2012.30948. PMC 3542482. PMID 23319969.
- ^ Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, Krause PJ, Bakken JS, Strle F, Stanek G, Bockenstedt L, Fish D, Dumler JS, Nadelman RB (November 2006). “The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America” (PDF). Clinical Infectious Diseases. 43 (9): 1089–134. doi:10.1086/508667. PMID 17029130. Archived (PDF) from the original on 27 November 2014.
- ^ Jump up to:a b Halperin JJ (June 2008). “Nervous system Lyme disease”. Infectious Disease Clinics of North America. 22 (2): 261–74, vi. doi:10.1016/j.idc.2007.12.009. PMID 18452800.
- ^ Jump up to:a b c d e f g h i j Mygland A, Ljøstad U, Fingerle V, Rupprecht T, Schmutzhard E, Steiner I (January 2010). “EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis” (PDF). European Journal of Neurology. 17 (1): 8–16. doi:10.1111/j.1468-1331.2009.02862.x. PMID 19930447. S2CID 14166137. Archived (PDF) from the original on 8 August 2017. Retrieved 30 April 2019.
- ^ Jump up to:a b c d e Pachner AR, Steere AC (July 1984). “Neurological findings of Lyme disease”. Yale Journal of Biology and Medicine. 57 (4): 481–3. PMC 2590042. PMID 6516450.
- ^ Jump up to:a b c d e f g h Ogrinc K, Lusa L, Lotrič-Furlan S, Bogovič P, Stupica D, Cerar T, Ružić-Sabljić E, Strle F (August 2016). “Course and outcome of early European Lyme neuroborreliosis (Bannwarth syndrome): clinical and laboratory findings”. Clinical Infectious Diseases. 63 (3): 346–53. doi:10.1093/cid/ciw299. PMID 27161773.
- ^ Jump up to:a b c d e f g h i Garro A, Nigrovic LE (May 2018). “Managing Peripheral Facial Palsy”. Annals of Emergency Medicine. 71 (5): 618–623. doi:10.1016/j.annemergmed.2017.08.039. PMID 29110887.
- ^ Jump up to:a b Halperin JJ (September 2010). “Nervous system Lyme disease”. J R Coll Physicians Edinb. 40 (3): 248–55. doi:10.4997/JRCPE.2010.314. PMID 21127770.
- ^ Jump up to:a b c d e f g h i j k l m n o Fish AE, Pride YB, Pinto DS (June 2008). “Lyme carditis” (PDF). Infect Dis Clin North Am. 22 (2): 275–88. doi:10.1016/j.idc.2007.12.008. PMID 18452801. Archived (PDF) from the original on 29 August 2017. Retrieved 9 May 2019.
- ^ Jump up to:a b Stanek G, Wormser GP, Gray J, Strle F (February 2012). “Lyme borreliosis”. Lancet. 379 (9814): 461–73. doi:10.1016/S0140-6736(11)60103-7. PMID 21903253. S2CID 31461047.
- ^ Jump up to:a b Stanek G, Strle F (June 2008). “Lyme disease: European perspective”. Infectious Disease Clinics of North America. 22 (2): 327–39, vii. doi:10.1016/j.idc.2008.01.001. PMID 18452805.
- ^ Puius YA, Kalish RA (June 2008). “Lyme arthritis: pathogenesis, clinical presentation, and management”. Infectious Disease Clinics of North America. 22 (2): 289–300, vi–vii. doi:10.1016/j.idc.2007.12.014. PMID 18452802.
- ^ Jump up to:a b Auwaerter PG, Aucott J, Dumler JS (January 2004). “Lyme borreliosis (Lyme disease): molecular and cellular pathobiology and prospects for prevention, diagnosis and treatment”. Expert Reviews in Molecular Medicine. 6(2): 1–22. doi:10.1017/S1462399404007276. PMID 14987414.
- ^ Bratton RL, Whiteside JW, Hovan MJ, Engle RL, Edwards FD (May 2008). “Diagnosis and treatment of Lyme disease”. Mayo Clinic Proceedings. 83(5): 566–571. doi:10.4065/83.5.566. PMID 18452688.
- ^ Shadick NA, Phillips CB, Sangha O, Logigian EL, Kaplan RF, Wright EA, Fossel AH, Fossel K, Berardi V, Lew RA, Liang MH (December 1999). “Musculoskeletal and neurologic outcomes in patients with previously treated Lyme disease”. Annals of Internal Medicine. 131 (12): 919–26. doi:10.7326/0003-4819-131-12-199912210-00003. PMID 10610642. S2CID 20746489.
- ^ Seltzer EG, Gerber MA, Cartter ML, Freudigman K, Shapiro ED (February 2000). “Long-term outcomes of persons with Lyme disease”. JAMA. 283 (5): 609–16. doi:10.1001/jama.283.5.609. PMID 10665700.
- ^ Fallon BA, Nields JA (November 1994). “Lyme disease: a neuropsychiatric illness”. The American Journal of Psychiatry. 151 (11): 1571–83. doi:10.1176/ajp.151.11.1571. PMID 7943444. S2CID 22568915.
- ^ Hess A, Buchmann J, Zettl UK, Henschel S, Schlaefke D, Grau G, Benecke R (March 1999). “Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder”. Biological Psychiatry. 45(6): 795. doi:10.1016/S0006-3223(98)00277-7. PMID 10188012. S2CID 44486654.
- ^ Mullegger RR (2004). “Dermatological manifestations of Lyme borreliosis”. European Journal of Dermatology. 14 (5): 296–309. PMID 15358567.
- ^ Samuels DS, Radolf JD, eds. (2010). “Chapter 6, Structure, Function and Biogenesis of the Borrelia Cell Envelope”. Borrelia: Molecular Biology, Host Interaction and Pathogenesis. Caister Academic Press. ISBN 978-1-904455-58-5.
- ^ Cutler SJ, Ruzic-Sabljic E, Potkonjak A (February 2017). “Emerging borreliae – Expanding beyond Lyme borreliosis” (PDF). Molecular and Cellular Probes. 31: 22–27. doi:10.1016/j.mcp.2016.08.003. PMID 27523487. Archived (PDF) from the original on 20 July 2018. Retrieved 5 July 2019.
- ^ Stanek G, Reiter M (April 2011). “The expanding Lyme Borrelia complex–clinical significance of genomic species?”. Clinical Microbiology and Infection. 17 (4): 487–93. doi:10.1111/j.1469-0691.2011.03492.x. PMID 21414082.
- ^ Schneider BS, Schriefer ME, Dietrich G, Dolan MC, Morshed MG, Zeidner NS (October 2008). “Borrelia bissettii isolates induce pathology in a murine model of disease”. Vector Borne and Zoonotic Diseases. 8 (5): 623–33. doi:10.1089/vbz.2007.0251. PMID 18454594. Archived from the original on 29 January 2020. Retrieved 29 January 2020.
- ^ Rudenko N, Golovchenko M, Mokrácek A, Piskunová N, Ruzek D, Mallatová N, Grubhoffer L (October 2008). “Detection of Borrelia bissettii in cardiac valve tissue of a patient with endocarditis and aortic valve stenosis in the Czech Republic”. Journal of Clinical Microbiology. 46 (10): 3540–3. doi:10.1128/JCM.01032-08. PMC 2566110. PMID 18650352.
- ^ Jump up to:a b Tilly K, Rosa PA, Stewart PE (June 2008). “Biology of infection with Borrelia burgdorferi”. Infectious Disease Clinics of North America. 22 (2): 217–34, v. doi:10.1016/j.idc.2007.12.013. PMC 2440571. PMID 18452798.
- ^ Jump up to:a b c d Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology(4th ed.). McGraw Hill. pp. 434–37. ISBN 978-0-8385-8529-0.
- ^ 2005 Fact Sheet, Prevent Tick Bites: Prevent Lyme Disease Archived26 June 2013 at the Wayback Machine, Rutgers University, Rutgers Cooperative Research & Extension, New Jersey Agricultural Experiment Station, Deborah Smith-Fiola, Former Ocean County Agricultural Agent and George C. Hamilton, PhD, Extension Specialist in Pest Management, March 2005.
- ^ People are freaking out over the CDC’s photo of a muffin with ticks in itArchived 25 January 2020 at the Wayback Machine, Deseret News (Utah), Herb Scribner, 31 May 2019. The U.S. CDC published a picture of a poppy seed muffin in which some of the “poppy seeds” were actually ticks.
- ^ Jump up to:a b Lo Re V, Occi JL, MacGregor RR (April 2004). “Identifying the vector of Lyme disease”. American Family Physician. 69 (8): 1935–7. PMID 15117014.
- ^ “Westport Weston Health District”. 2004. Archived from the original on 29 September 2013. Retrieved 26 September 2013.
- ^ Jump up to:a b “Lyme Disease Data and surveillance”. Lyme Disease. Centers for Disease Control and Prevention. 5 February 2019. Archived from the original on 13 April 2019. Retrieved 12 April 2019.
- ^ Hovius JW, van Dam AP, Fikrig E (September 2007). “Tick-host-pathogen interactions in Lyme borreliosis” (PDF). Trends in Parasitology. 23 (9): 434–8. doi:10.1016/j.pt.2007.07.001. PMID 17656156. Archived (PDF) from the original on 16 February 2019. Retrieved 9 September 2019.
- ^ Jump up to:a b c Steere AC, Coburn J, Glickstein L (April 2004). “The emergence of Lyme disease”. The Journal of Clinical Investigation. 113 (8): 1093–101. doi:10.1172/JCI21681. PMC 385417. PMID 15085185.
- ^ Hu, Linden (13 May 2019). “Patient education: What to do after a tick bite to prevent Lyme disease (Beyond the Basics)”. www.uptodate.com. UpToDate. Archived from the original on 1 January 2020. Retrieved 30 January 2020.
- ^ de Mik EL, van Pelt W, Docters-van Leeuwen BD, van der Veen A, Schellekens JF, Borgdorff MW (April 1997). “The geographical distribution of tick bites and erythema migrans in general practice in The Netherlands”. International Journal of Epidemiology. 26 (2): 451–7. doi:10.1093/ije/26.2.451. PMID 9169184.
- ^ Sun Y, Xu R (2003). “Ability of Ixodes persulcatus, Haemaphysalis concinna and Dermacentor silvarum ticks to acquire and transstadially transmit Borrelia garinii”. Experimental & Applied Acarology. 31 (1–2): 151–60. doi:10.1023/B:APPA.0000005119.30172.43. PMID 14756409. S2CID 19214181.
- ^ Ledin KE, Zeidner NS, Ribeiro JM, Biggerstaff BJ, Dolan MC, Dietrich G, Vredevoe L, Piesman J (March 2005). “Borreliacidal activity of saliva of the tick Amblyomma americanum”. Medical and Veterinary Entomology. 19 (1): 90–5. doi:10.1111/j.0269-283X.2005.00546.x. PMID 15752182. S2CID 270178.
- ^ Masters EJ, Grigery CN, Masters RW (June 2008). “STARI, or Masters disease: Lone Star tick-vectored Lyme-like illness”. Infectious Disease Clinics of North America. 22 (2): 361–76, viii. doi:10.1016/j.idc.2007.12.010. PMID 18452807.
- ^ Clark K (November 2004). “Borrelia species in host-seeking ticks and small mammals in northern Florida”. Journal of Clinical Microbiology. 42 (11): 5076–86. doi:10.1128/JCM.42.11.5076-5086.2004. PMC 525154. PMID 15528699.
- ^ Eisen L, Eisen RJ, Lane RS (December 2004). “The roles of birds, lizards, and rodents as hosts for the western black-legged tick Ixodes pacificus”. Journal of Vector Ecology. 29 (2): 295–308. PMID 15709249.
- ^ Jump up to:a b Lane RS, Mun J, Eisen L, Eisen RJ (August 2006). “Refractoriness of the western fence lizard (Sceloporus occidentalis) to the Lyme disease group spirochete Borrelia bissettii”. The Journal of Parasitology. 92 (4): 691–6. doi:10.1645/GE-738R1.1. PMID 16995383. S2CID 24200639.
- ^ Walsh CA, Mayer EW, Baxi LV (January 2007). “Lyme disease in pregnancy: case report and review of the literature”. Obstetrical & Gynecological Survey. 62 (1): 41–50. doi:10.1097/01.ogx.0000251024.43400.9a. PMID 17176487. S2CID 31929160.
- ^ Dotters-Katz, S; Kuller, J; Heine, P (September 2013). “Arthropod-Borne Bacterial Diseases in Pregnancy”. Obstetrical & Gynecological Survey. 68 (9): 41–50. doi:10.1097/OGX.0b013e3182a5ed46. PMID 25102120. S2CID 26801402.
- ^ Lakos A, Solymosi N (June 2010). “Maternal Lyme borreliosis and pregnancy outcome”. International Journal of Infectious Diseases. 14 (6): e494–8. doi:10.1016/j.ijid.2009.07.019. PMID 19926325.
- ^ Steere A (31 August 1989). “Medical Progress, Lyme Disease”. The New England Journal of Medicine. 321 (9): 586–596. doi:10.1056/NEJM198908313210906. PMID 2668764.
- ^ “Tick Attachment and Tickborne Diseases”. www.maine.gov. Archivedfrom the original on 1 October 2018. Retrieved 1 October 2018.
- ^ Magnarelli LA, Anderson JF (August 1988). “Ticks and biting insects infected with the etiologic agent of Lyme disease, Borrelia burgdorferi”. Journal of Clinical Microbiology. 26 (8): 1482–6. doi:10.1128/jcm.26.8.1482-1486.1988. PMC 266646. PMID 3170711.
- ^ Luger SW (June 1990). “Lyme disease transmitted by a biting fly”. The New England Journal of Medicine. 322 (24): 1752. doi:10.1056/NEJM199006143222415. PMID 2342543.
- ^ Bach G (2001). “Recovery of Lyme spirochetes by PCR in semen samples of previously diagnosed Lyme disease patients”. 14th International Scientific Conference on Lyme Disease. Archived from the original on 20 June 2006.
- ^ Schmidt BL, Aberer E, Stockenhuber C, Klade H, Breier F, Luger A (March 1995). “Detection of Borrelia burgdorferi DNA by polymerase chain reaction in the urine and breast milk of patients with Lyme borreliosis”. Diagnostic Microbiology and Infectious Disease. 21 (3): 121–8. doi:10.1016/0732-8893(95)00027-8. PMID 7648832.
- ^ “CDC Lyme FAQ”. Centers for Disease Control. 19 July 2018. Archivedfrom the original on 26 March 2013.
- ^ Swanson SJ, Neitzel D, Reed KD, Belongia EA (October 2006). “Coinfections acquired from ixodes ticks”. Clinical Microbiology Reviews. 19(4): 708–27. doi:10.1128/CMR.00011-06. PMC 1592693. PMID 17041141.
- ^ Wormser GP (June 2006). “Clinical practice. Early Lyme disease”. The New England Journal of Medicine. 354 (26): 2794–801. doi:10.1056/NEJMcp061181. PMID 16807416.
- ^ Lindgren E, Gustafson R (July 2001). “Tick-borne encephalitis in Sweden and climate change”. Lancet. 358 (9275): 16–8. doi:10.1016/S0140-6736(00)05250-8. PMID 11454371. S2CID 336323.
- ^ Varde S, Beckley J, Schwartz I (1998). “Prevalence of tick-borne pathogens in Ixodes scapularis in a rural New Jersey County”. Emerging Infectious Diseases. 4 (1): 97–9. doi:10.3201/eid0401.980113. PMC 2627663. PMID 9452402.
- ^ Pachner AR, Steiner I (June 2007). “Lyme neuroborreliosis: infection, immunity, and inflammation”. The Lancet. Neurology. 6 (6): 544–52. doi:10.1016/S1474-4422(07)70128-X. PMID 17509489. S2CID 11600373.
- ^ Fikrig E, Narasimhan S (April 2006). “Borrelia burgdorferi–traveling incognito?”. Microbes and Infection. 8 (5): 1390–9. doi:10.1016/j.micinf.2005.12.022. PMID 16698304.
- ^ Xu Q, Seemanapalli SV, Reif KE, Brown CR, Liang FT (April 2007). “Increasing the recruitment of neutrophils to the site of infection dramatically attenuates Borrelia burgdorferi infectivity”. Journal of Immunology. 178 (8): 5109–15. doi:10.4049/jimmunol.178.8.5109. PMID 17404293.
- ^ Coleman JL, Gebbia JA, Piesman J, Degen JL, Bugge TH, Benach JL (June 1997). “Plasminogen is required for efficient dissemination of B. burgdorferi in ticks and for enhancement of spirochetemia in mice”. Cell. 89 (7): 1111–9. doi:10.1016/S0092-8674(00)80298-6. PMID 9215633. S2CID 18750257.
- ^ Steere AC (July 2001). “Lyme disease”. The New England Journal of Medicine. 345 (2): 115–25. doi:10.1056/NEJM200107123450207. PMID 11450660.
- ^ Rupprecht TA, Koedel U, Fingerle V, Pfister HW (2008). “The pathogenesis of lyme neuroborreliosis: from infection to inflammation”. Molecular Medicine. 14 (3–4): 205–12. doi:10.2119/2007-00091.Rupprecht. PMC 2148032. PMID 18097481. Archived from the original on 3 April 2015.
- ^ Cabello FC, Godfrey HP, Newman SA (August 2007). “Hidden in plain sight: Borrelia burgdorferi and the extracellular matrix”. Trends in Microbiology. 15(8): 350–4. doi:10.1016/j.tim.2007.06.003. PMID 17600717. Archivedfrom the original on 7 July 2019. Retrieved 5 July 2019.
- ^ Ramesh G, Alvarez AL, Roberts ED, Dennis VA, Lasater BL, Alvarez X, Philipp MT (September 2003). “Pathogenesis of Lyme neuroborreliosis: Borrelia burgdorferi lipoproteins induce both proliferation and apoptosis in rhesus monkey astrocytes”. European Journal of Immunology. 33 (9): 2539–50. doi:10.1002/eji.200323872. PMID 12938230. S2CID 25448372.
- ^ Halperin JJ, Heyes MP (January 1992). “Neuroactive kynurenines in Lyme borreliosis”. Neurology. 42 (1): 43–50. doi:10.1212/WNL.42.1.43. PMID 1531156. S2CID 37495839.
- ^ Fallon BA, Keilp J, Prohovnik I, Heertum RV, Mann JJ (2003). “Regional cerebral blood flow and cognitive deficits in chronic lyme disease”. The Journal of Neuropsychiatry and Clinical Neurosciences. 15 (3): 326–32. doi:10.1176/appi.neuropsych.15.3.326. PMID 12928508.
- ^ Gasse T, Murr C, Meyersbach P, Schmutzhard E, Wachter H, Fuchs D (September 1994). “Neopterin production and tryptophan degradation in acute Lyme neuroborreliosis versus late Lyme encephalopathy”. European Journal of Clinical Chemistry and Clinical Biochemistry (Submitted manuscript). 32 (9): 685–9. doi:10.1515/cclm.1994.32.9.685. PMID 7865624. S2CID 22214184.
- ^ Zajkowska J, Grygorczuk S, Kondrusik M, Pancewicz S, Hermanowska-Szpakowicz T (2006). “[New aspects of pathogenesis of Lyme borreliosis]”. Przeglad Epidemiologiczny (in Polish). 60 Suppl 1 (Suppl 1): 167–70. PMID 16909797.
- ^ Ercolini AM, Miller SD (January 2009). “The role of infections in autoimmune disease”. Clinical and Experimental Immunology. 155 (1): 1–15. doi:10.1111/j.1365-2249.2008.03834.x. PMC 2665673. PMID 19076824.
- ^ Singh SK, Girschick HJ (July 2004). “Lyme borreliosis: from infection to autoimmunity”. Clinical Microbiology and Infection. 10 (7): 598–614. doi:10.1111/j.1469-0691.2004.00895.x. PMID 15214872.
- ^ Oldstone MB (October 1998). “Molecular mimicry and immune-mediated diseases”. FASEB Journal. 12 (13): 1255–65. doi:10.1096/fasebj.12.13.1255. PMC 7164021. PMID 9761770. S2CID 16089636.
- ^ Raveche ES, Schutzer SE, Fernandes H, Bateman H, McCarthy BA, Nickell SP, Cunningham MW (February 2005). “Evidence of Borrelia autoimmunity-induced component of Lyme carditis and arthritis”. Journal of Clinical Microbiology. 43 (2): 850–6. doi:10.1128/JCM.43.2.850-856.2005. PMC 548028. PMID 15695691.
- ^ Weinstein A, Britchkov M (July 2002). “Lyme arthritis and post-Lyme disease syndrome”. Current Opinion in Rheumatology. 14 (4): 383–7. doi:10.1097/00002281-200207000-00008. PMID 12118171.
- ^ Bolz DD, Weis JJ (August 2004). “Molecular mimicry to Borrelia burgdorferi: pathway to autoimmunity?”. Autoimmunity. 37 (5): 387–92. doi:10.1080/08916930410001713098. PMID 15621562. S2CID 43045224.
- ^ Brown SL, Hansen SL, Langone JJ (July 1999). “Role of serology in the diagnosis of Lyme disease”. JAMA. 282 (1): 62–6. doi:10.1001/jama.282.1.62. PMID 10404913.
- ^ Hofmann H (1996). “Lyme borreliosis—problems of serological diagnosis”. Infection. 24 (6): 470–2. doi:10.1007/BF01713052. PMID 9007597. S2CID 19701481.
- ^ Wormser GP, Masters E, Nowakowski J, McKenna D, Holmgren D, Ma K, Ihde L, Cavaliere LF, Nadelman RB (October 2005). “Prospective clinical evaluation of patients from Missouri and New York with erythema migrans-like skin lesions”. Clinical Infectious Diseases. 41 (7): 958–65. doi:10.1086/432935. PMID 16142659.
- ^ Jump up to:a b “Lyme Disease risk areas map”. Risk of Lyme disease to Canadians. Government of Canada. 27 January 2015. Archived from the original on 10 May 2019. Retrieved 8 May 2019.
- ^ Jump up to:a b c d e f Aucott J, Morrison C, Munoz B, Rowe PC, Schwarzwalder A, West SK (1 June 2009). “Diagnostic challenges of early Lyme disease: Lessons from a community case series”. BMC Infectious Diseases. 9 (79): 79. doi:10.1186/1471-2334-9-79. PMC 2698836. PMID 19486523.
- ^ “Lyme disease diagnosis”. Centers for Disease Control and Prevention(CDC). 7 October 2008. Archived from the original on 28 August 2009. Retrieved 6 July 2009.
- ^ Jump up to:a b “Lyme disease”. NICE guideline [NG95]. National Institute for Health and Care Excellence. Archived from the original on 11 May 2019. Retrieved 24 May 2019.
- ^ Wilske B (2005). “Epidemiology and diagnosis of Lyme borreliosis”. Annals of Medicine. 37 (8): 568–79. doi:10.1080/07853890500431934. PMID 16338759. S2CID 30818459.
- ^ Jump up to:a b c Depietropaolo DL, Powers, JH, Gill JM, Foy AJ (15 July 2005). “Diagnosis of Lyme disease”. American Family Physician. 72 (2): 297–305. doi:10.1093/cid/cir464. PMID 16050454.
- ^ “Are serological tests of any value in the diagnosis of Lyme disease?”. American Lyme Disease Foundation. Archived from the original on 19 December 2019. Retrieved 2 December 2019.
- ^ Coyle PK, Schutzer SE, Deng Z, Krupp LB, Belman AL, Benach JL, Luft BJ (November 1995). “Detection of Borrelia burgdorferi-specific antigen in antibody-negative cerebrospinal fluid in neurologic Lyme disease”. Neurology. 45 (11): 2010–5. doi:10.1212/WNL.45.11.2010. PMID 7501150. S2CID 23797801.
- ^ Jump up to:a b c d Halperin JJ, Shapiro ED, Logigian E, Belman AL, Dotevall L, Wormser GP, Krupp L, Gronseth G, Bever CT (July 2007). “Practice parameter: treatment of nervous system Lyme disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology”. Neurology. 69 (1): 91–102. doi:10.1212/01.wnl.0000265517.66976.28. PMID 17522387.
- ^ Molloy PJ, Persing DH, Berardi VP (August 2001). “False-positive results of PCR testing for Lyme disease”. Clinical Infectious Diseases. 33 (3): 412–3. doi:10.1086/321911. PMID 11438915.
- ^ Jump up to:a b Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser GP (July 2005). “Diagnosis of lyme borreliosis”. Clinical Microbiology Reviews. 18 (3): 484–509. doi:10.1128/CMR.18.3.484-509.2005. PMC 1195970. PMID 16020686.
- ^ Nocton JJ, Dressler F, Rutledge BJ, Rys PN, Persing DH, Steere AC (January 1994). “Detection of Borrelia burgdorferi DNA by polymerase chain reaction in synovial fluid from patients with Lyme arthritis”. The New England Journal of Medicine. 330 (4): 229–34. doi:10.1056/NEJM199401273300401. PMID 8272083.
- ^ Hyde FW, Johnson RC, White TJ, Shelburne CE (January 1989). “Detection of antigens in urine of mice and humans infected with Borrelia burgdorferi, etiologic agent of Lyme disease”. Journal of Clinical Microbiology. 27 (1): 58–61. doi:10.1128/JCM.27.1.58-61.1989. PMC 267232. PMID 2913036.
- ^ Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, Liotta L, Narayanan A, Lepene B, Kehn-Hall K (July 2014). “The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics”. Pathogens and Disease. 71 (2): 164–76. doi:10.1111/2049-632X.12136. PMC 7108521. PMID 24449537.
- ^ Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, Liotta L, Narayanan A, Lepene B, Kehn-Hall K (July 2014). “The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics”. Pathogens and Disease. 71 (2): 164–76. doi:10.1111/2049-632x.12136. PMID 24449537.
- ^ Burdash N, Fernandes J (June 1991). “Lyme borreliosis: detecting the great imitator”. The Journal of the American Osteopathic Association. 91 (6): 573–4, 577–8. PMID 1874654.
- ^ Hildenbrand P, Craven DE, Jones R, Nemeskal P (June 2009). “Lyme neuroborreliosis: manifestations of a rapidly emerging zoonosis”. AJNR. American Journal of Neuroradiology. 30 (6): 1079–87. doi:10.3174/ajnr.A1579. PMC 7051319. PMID 19346313.
- ^ Westervelt HJ, McCaffrey RJ (September 2002). “Neuropsychological functioning in chronic Lyme disease”. Neuropsychology Review. 12 (3): 153–77. doi:10.1023/A:1020381913563. PMID 12428915. S2CID 2807397.
- ^ Dworkin RH, Johnson RW, Breuer J, et al. (2007). “Recommendations for the management of herpes zoster”. Clin. Infect. Dis. 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845. S2CID 10894629.
- ^ Halperin JJ (May 2015). “Chronic Lyme disease: misconceptions and challenges for patient management”. Infection and Drug Resistance. 8: 119–128. doi:10.2147/IDR.S66739. PMC 4440423. PMID 26028977.
- ^ Jump up to:a b Tarulli AW, Raynor EM (May 2007). “Lumbosacral radiculopathy”(PDF). Neurologic Clinics. 25 (2): 387–405. doi:10.1016/j.ncl.2007.01.008. PMID 17445735. S2CID 15518713.
- ^ Pachner AR (1989). “Neurologic manifestations of Lyme disease, the new “great imitator““. Reviews of Infectious Diseases. 11 Suppl 6: S1482–6. doi:10.1093/clinids/11.Supplement_6.S1482. PMID 2682960. S2CID 3862308.
- ^ Branda JA, Linskey K, Kim YA, Steere AC, Ferraro MJ (September 2011). “Two-tiered antibody testing for Lyme disease with use of 2 enzyme immunoassays, a whole-cell sonicate enzyme immunoassay followed by a VlsE C6 peptide enzyme immunoassay”. Clinical Infectious Diseases. 53 (6): 541–7. doi:10.1093/cid/cir464. PMID 21865190.
- ^ Jump up to:a b c d e f g h i j “Preventing tick bites on people”. Lyme Disease. Centers for Disease Control and Prevention. 8 March 2019. Archived from the original on 15 June 2019. Retrieved 21 May 2019.
- ^ Jump up to:a b “About ticks – preventative measures”. Tick-borne diseases. Companion Vector-Borne Diseases. Archived from the original on 7 June 2019. Retrieved 21 May 2019.
- ^ Jump up to:a b c d e f Eisen L, Eisen RJ (September 2016). “Critical evaluation of the linkage between tick-based risk measures and the occurrence of Lyme disease cases”. J Med Entomol. 53 (5): 1050–1062. doi:10.1093/jme/tjw092. PMC 5777907. PMID 27330093.
- ^ “Host seeking”. CVBD: Companion Vector-Borne Diseases. Archivedfrom the original on 16 October 2016. Retrieved 8 December 2016.
- ^ Jump up to:a b c “Tips to prevent tick bytes”. Insect repellents. Environmental Protection Agency. 15 July 2013. Archived from the original on 15 April 2019. Retrieved 21 May 2019.
- ^ Jump up to:a b c d e f g h “Protection against Mosquitoes, Ticks, & Other Arthropods”. Travelers’ Health. Centers for Disease Control and Prevention. Archivedfrom the original on 9 May 2019. Retrieved 21 May 2019.
- ^ Jump up to:a b c Miller NJ, Rainone EE, Dyer MC, González ML, Mather TN (March 2011). “Tick bite protection with permethrin-treated summer-weight clothing”. J Med Entomol. 48 (2): 327–33. doi:10.1603/me10158. PMID 21485369.
- ^ Jump up to:a b Eisen L, Rose D, Prose R, Breuner NE, Dolan MC, Thompson K, Connally N (October 2017). “Bioassays to evaluate non-contact spatial repellency, contact irritancy and acute toxicity of permethrin-treated clothing against nymphal Ixodes scapularis ticks”. Ticks Tick Borne Dis. 8 (6): 837–49. doi:10.1016/j.ttbdis.2017.06.010. PMC 5665650. PMID 28754599.
- ^ Dymond NL, Swift IM (June 2008). “Permethrin toxicity in cats: a retrospective study of 20 cases”. Aust Vet J. 86 (6): 219–23. doi:10.1111/j.1751-0813.2008.00298.x. PMID 18498556.
- ^ Jump up to:a b “Repellents: protection against mosquitoes, ticks and other arthropods”. Insect repellents. Environmental Protection Agency. 9 July 2013. Archivedfrom the original on 20 May 2019. Retrieved 21 May 2019.
- ^ Jump up to:a b c Nguyen QD, Vu MN, Hebert AA (November 2018). “Insect repellents: an updated review for the clinician”. J Am Acad Dermatol. doi:10.1016/j.jaad.2018.10.053. PMID 30395919.
- ^ Jump up to:a b c d e Stafford KC (2007). “Tick management handbook (rev. ed.)”(PDF). Bulletins. Connecticut Agricultural Experiment Station. Archived(PDF) from the original on 3 April 2019. Retrieved 21 May 2019.
- ^ Piesman J, Dolan MC (May 2002). “Protection against lyme disease spirochete transmission provided by prompt removal of nymphal Ixodes scapularis (Acari: Ixodidae)”. Journal of Medical Entomology. 39 (3): 509–12. doi:10.1603/0022-2585-39.3.509. PMID 12061448. S2CID 39805040.
- ^ Jump up to:a b c d e f “Tick removal and testing”. Lyme Disease. Centers for Disease Control and Prevention. 22 April 2019. Archived from the original on 23 November 2017. Retrieved 21 May 2019.
- ^ Jump up to:a b “Tick Allergy”. 2014. Archived from the original on 14 May 2015. Retrieved 30 April 2015.
- ^ Duggal N, Luo E (May 2017). “Cryotherapy: Is Freezing Warts an Effective Treatment?”. Healthline. Archived from the original on 4 September 2017. Retrieved 21 May 2019.
- ^ Celenza A, Rogers IR (2002). “The “Knot Method” of Tick Removal”. Wilderness & Environmental Medicine. 13 (2): 179–180. doi:10.1580/1080-6032(2002)013[0181:ltte]2.0.co;2. PMID 12092975.
- ^ Ghirga, Giovanni; Ghirga, Paolo (1 September 2010). “Effective Tick Removal With a Fishing Line Knot”. Wilderness & Environmental Medicine. 21 (3): 270–271. doi:10.1016/j.wem.2010.04.005. ISSN 1080-6032. PMID 20832708.
- ^ Jump up to:a b c d e “Preventing tick bites in the yard”. Lyme Disease. Centers for Disease Control and Prevention. 8 March 2019. Archived from the original on 15 June 2019. Retrieved 21 May 2019.
- ^ “CDC – Lyme Disease – NIOSH Workplace Safety and Health Topic”. www.cdc.gov. 3 August 2017. Archived from the original on 13 November 2015. Retrieved 3 November 2015.
- ^ “Risks: Lyme Disease | NIOSH | CDC”. www.cdc.gov. 14 November 2018. Archived from the original on 26 April 2019. Retrieved 26 April 2019.
- ^ “Lyme disease”. The Centers for Disease Control and Prevention. 12 October 2016. Archived from the original on 17 June 2017. Retrieved 22 June 2017.
 This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention. - ^ Rand PW, Lubelczyk C, Holman MS, Lacombe EH, Smith RP (July 2004). “Abundance of Ixodes scapularis (Acari: Ixodidae) after the complete removal of deer from an isolated offshore island, endemic for Lyme Disease”. Journal of Medical Entomology. 41 (4): 779–84. doi:10.1603/0022-2585-41.4.779. PMID 15311475. S2CID 5853201.
- ^ “Figure 2: Changes in deer density and cases of Lyme disease in Mumford Cove, Connecticut, 1996–2004 (CT DEP data)” (PDF). Managing Urban Deer in Connecticut (2nd ed.). Connecticut Department of Environmental Protection – Wildlife Division. June 2007. p. 4. Archived (PDF) from the original on 2 June 2013.
- ^ Perkins SE, Cattadori IM, Tagliapietra V, Rizzoli AP, Hudson PJ (August 2006). “Localized deer absence leads to tick amplification”. Ecology. 87 (8): 1981–6. CiteSeerX 10.1.1.218.7660. doi:10.1890/0012-9658(2006)87[1981:LDALTT]2.0.CO;2. PMID 16937637.
- ^ Stafford, Kirby C. (2004). Tick Management Handbook (PDF). Connecticut Agricultural Experiment Station and Connecticut Department of Public Health. p. 46. Archived (PDF) from the original on 25 October 2007. Retrieved 21 August 2007.
- ^ Jump up to:a b Gern L, Estrada-Peña A, Frandsen F, Gray JS, Jaenson TG, Jongejan F, Kahl O, Korenberg E, Mehl R, Nuttall PA (March 1998). “European reservoir hosts of Borrelia burgdorferi sensu lato”. Zentralblatt für Bakteriologie. 287 (3): 196–204. doi:10.1016/S0934-8840(98)80121-7. PMID 9580423.
- ^ Jump up to:a b Wodecka, Beata; Rymaszewska, Anna; Skotarczak, Bogumila (2013). “Host and pathogen DNA identification in blood meals of nymphal Ixodes ricinus ticks from forest parks and rural forests of Poland”. Experimental and Applied Acarology. 62 (4): 543–555. doi:10.1007/s10493-013-9763-x. PMC 3933768. PMID 24352572.
- ^ Jaenson TG, Tälleklint L (September 1992). “Incompetence of roe deer as reservoirs of the Lyme borreliosis spirochete”. Journal of Medical Entomology. 29 (5): 813–7. doi:10.1093/jmedent/29.5.813. PMID 1404260.
- ^ Tälleklint L, Jaenson TG (1994). “Transmission of Borrelia burgdorferi s.l. from mammal reservoirs to the primary vector of Lyme borreliosis, Ixodes ricinus (Acari: Ixodidae), in Sweden”. Journal of Medical Entomology. 31 (6): 880–886. doi:10.1093/jmedent/31.6.880. PMID 7815401.
- ^ Jump up to:a b Wodecka B, Rymaszewska A, Skotarczak B (April 2014). “Host and pathogen DNA identification in blood meals of nymphal Ixodes ricinus ticks from forest parks and rural forests of Poland”. Experimental & Applied Acarology. 62 (4): 543–55. doi:10.1007/s10493-013-9763-x. PMC 3933768. PMID 24352572.
- ^ Overzier E, Pfister K, Herb I, Mahling M, Böck G, Silaghi C (June 2013). “Detection of tick-borne pathogens in roe deer (Capreolus capreolus), in questing ticks (Ixodes ricinus), and in ticks infesting roe deer in southern Germany”. Ticks and Tick-Borne Diseases. 4 (4): 320–8. doi:10.1016/j.ttbdis.2013.01.004. PMID 23571115.
- ^ Poland GA, Jacobson RM (March 2001). “The prevention of Lyme disease with vaccine”. Vaccine. 19 (17–19): 2303–8. doi:10.1016/S0264-410X(00)00520-X. PMID 11257352.
- ^ Rowe, Claudia (13 June 1999). “Lukewarm Response To New Lyme Vaccine”. The New York Times. Archived from the original on 10 February 2012. Retrieved 11 July 2008.
- ^ Jump up to:a b c Abbott A (February 2006). “Lyme disease: uphill struggle”. Nature. 439 (7076): 524–5. doi:10.1038/439524a. PMID 16452949. S2CID 4315588.
- ^ “Sole Lyme Vaccine Is Pulled Off Market”. The New York Times. 28 February 2002. Archived from the original on 30 August 2010. Retrieved 11 July 2008.
- ^ Jump up to:a b Nigrovic LE, Thompson KM (January 2007). “The Lyme vaccine: a cautionary tale”. Epidemiology and Infection. 135 (1): 1–8. doi:10.1017/S0950268806007096. PMC 2870557. PMID 16893489.
- ^ Jump up to:a b Brooks, DVM, Wendy C. “Lyme Disease”. Veterinary Information Network. Archived from the original on 4 April 2015. Retrieved 10 February2012.
- ^ “Anti-vaxxers stopped the last Lyme disease vaccine. The FDA has just fast-tracked a new one”. Newsweek. 25 July 2017. Archived from the original on 25 December 2017. Retrieved 25 December 2017.
- ^ Berende A, ter Hofstede HJ, Vos FJ, van Middendorp H, Vogelaar ML, Tromp M, van den Hoogen FH, Donders AR, Evers AW, Kullberg BJ (March 2016). “Randomized Trial of Longer-Term Therapy for Symptoms Attributed to Lyme Disease”. The New England Journal of Medicine. 374 (13): 1209–20. doi:10.1056/NEJMoa1505425. PMID 27028911.
- ^ Michelle Stephenson (4 October 2012). “OTC Drops: Telling the Tears Apart”. Review of Ophtalmology. Jobson Medical Information LLC. Archived from the original on 17 April 2019. Retrieved 16 April 2019.
- ^ Jump up to:a b c d e Arvikar SL, Steere AC (June 2015). “Diagnosis and Treatment of Lyme Arthritis”. Infect Dis Clin North Am. 29 (2): 269–80. doi:10.1016/j.idc.2015.02.004. PMC 4443866. PMID 25999223.
- ^ Jump up to:a b c Wormser GP, Ramanathan R, Nowakowski J, McKenna D, Holmgren D, Visintainer P, Dornbush R, Singh B, Nadelman RB (May 2003). “Duration of antibiotic therapy for early Lyme disease. A randomized, double-blind, placebo-controlled trial”. Annals of Internal Medicine. 138 (9): 697–704. doi:10.7326/0003-4819-138-9-200305060-00005. PMID 12729423. S2CID 3083800.
- ^ Stupica D, Lusa L, Ruzić-Sabljić E, Cerar T, Strle F (August 2012). “Treatment of erythema migrans with doxycycline for 10 days versus 15 days”. Clin Infect Dis. 55 (3): 343–50. doi:10.1093/cid/cis402. PMID 22523260.
- ^ Jump up to:a b Dattwyler RJ, Luft BJ, Kunkel MJ, Finkel MF, Wormser GP, Rush TJ, Grunwaldt E, Agger WA, Franklin M, Oswald D, Cockey L, Maladorno D (July 1997). “Ceftriaxone compared with doxycycline for the treatment of acute disseminated Lyme disease”. New England Journal of Medicine. 337 (5): 289–94. doi:10.1056/NEJM199707313370501. PMID 9233865.
- ^ Vrethem M, Hellblom L, Widlund M, Ahl M, Danielsson O, Ernerudh J, Forsberg P (October 2002). “Chronic symptoms are common in patients with neuroborreliosis – a questionnaire follow-up study”. Acta Neurol Scand. 106(4): 205–8. doi:10.1034/j.1600-0404.2002.01358.x. PMID 12225315. S2CID 42290158.
- ^ Berglund J, Stjernberg L, Ornstein K, Tykesson-Joelsson K, Walter H (2002). “5-y Follow-up study of patients with neuroborreliosis”. Scand J Infect Dis. 34(6): 421–5. doi:10.1080/00365540110080421. PMID 12160168. S2CID 28306612.
- ^ Jump up to:a b c Clark JR, Carlson RD, Sasaki CT, Pachner AR, Steere AC (November 1985). “Facial paralysis in Lyme disease”. Laryngoscope. 95 (11): 1341–5. doi:10.1288/00005537-198511000-00009. PMID 4058212. S2CID 85021.
- ^ Jump up to:a b c Dotevall L, Hagberg L (March 1999). “Successful oral doxycycline treatment of Lyme disease-associated facial palsy and meningitis”. Clin Infect Dis. 28 (3): 569–74. doi:10.1086/515145. PMID 10194080.
- ^ Kalish RA, Kaplan RF, Taylor E, Jones-Woodward L, Workman K, Steere AC (February 2001). “Evaluation of study patients with Lyme disease, 10-20-year follow-up”. J Infect Dis. 183 (3): 453–60. doi:10.1086/318082. PMID 11133377.
- ^ Jump up to:a b c Jowett N, Gaudin RA, Banks CA, Hadlock TA (June 2017). “Steroid use in Lyme disease-associated facial palsy is associated with worse long-term outcomes”. Laryngoscope. 127 (6): 1451–8. doi:10.1002/lary.26273. PMID 27598389. S2CID 25596860.
- ^ Nadelman RB, Hanincová K, Mukherjee P, Liveris D, Nowakowski J, McKenna D, Brisson D, Cooper D, Bittker S, Madison G, Holmgren D, Schwartz I, Wormser GP (November 2012). “Differentiation of reinfection from relapse in recurrent Lyme disease”. N Engl J Med. 367 (20): 1883–90. doi:10.1056/NEJMoa1114362. PMC 3526003. PMID 23150958.
- ^ “Post-Treatment Lyme Disease Syndrome”. CDC. 3 November 2016. Archived from the original on 17 June 2017.
- ^ Higgins R (August 2004). “Emerging or re-emerging bacterial zoonotic diseases: bartonellosis, leptospirosis, Lyme borreliosis, plague”. Revue Scientifique et Technique. 23 (2): 569–81. doi:10.20506/rst.23.2.1503. PMID 15702720.
- ^ Bouattour A, Ghorbel A, Chabchoub A, Postic D (2004). “[Lyme borreliosis situation in North Africa]” [Lyme borreliosis situation in North Africa]. Archives de l’Institut Pasteur de Tunis (in French). 81 (1–4): 13–20. PMID 16929760.
- ^ Dsouli N, Younsi-Kabachii H, Postic D, Nouira S, Gern L, Bouattour A (July 2006). “Reservoir role of lizard Psammodromus algirus in transmission cycle of Borrelia burgdorferi sensu lato (Spirochaetaceae) in Tunisia” (PDF). Journal of Medical Entomology. 43 (4): 737–42. doi:10.1603/0022-2585(2006)43[737:RROLPA]2.0.CO;2. PMID 16892633. Archived(PDF) from the original on 19 July 2018. Retrieved 5 July 2019.
- ^ Helmy N (August 2000). “Seasonal abundance of Ornithodoros (O.) savignyi and prevalence of infection with Borrelia spirochetes in Egypt”. Journal of the Egyptian Society of Parasitology. 30 (2): 607–19. PMID 10946521.
- ^ Fivaz BH, Petney TN (September 1989). “Lyme disease–a new disease in southern Africa?”. Journal of the South African Veterinary Association. 60 (3): 155–8. PMID 2699499.
- ^ Jowi JO, Gathua SN (May 2005). “Lyme disease: report of two cases”. East African Medical Journal. 82 (5): 267–9. doi:10.4314/eamj.v82i5.9318. PMID 16119758.
- ^ Li M, Masuzawa T, Takada N, Ishiguro F, Fujita H, Iwaki A, Wang H, Wang J, Kawabata M, Yanagihara Y (July 1998). “Lyme disease Borrelia species in northeastern China resemble those isolated from far eastern Russia and Japan”. Applied and Environmental Microbiology. 64 (7): 2705–9. doi:10.1128/AEM.64.7.2705-2709.1998. PMC 106449. PMID 9647853.
- ^ Masuzawa T (December 2004). “Terrestrial distribution of the Lyme borreliosis agent Borrelia burgdorferi sensu lato in East Asia”. Japanese Journal of Infectious Diseases. 57 (6): 229–35. PMID 15623946. Archivedfrom the original on 22 January 2013.
- ^ Walder G, Lkhamsuren E, Shagdar A, et al. (May 2006). “Serological evidence for tick-borne encephalitis, borreliosis, and human granulocytic anaplasmosis in Mongolia”. International Journal of Medical Microbiology. 296 Suppl 40: 69–75. doi:10.1016/j.ijmm.2006.01.031. PMID 16524782.
- ^ Rizzoli A, Hauffe H, Carpi G, Vourc HG, Neteler M, Rosa R (July 2011). “Lyme borreliosis in Europe”. Euro Surveillance. 16 (27). PMID 21794218. Archived from the original on 9 July 2011.
- ^ Smith R, Takkinen J (June 2006). “Lyme borreliosis: Europe-wide coordinated surveillance and action needed?”. Euro Surveillance. 11 (6): E060622.1. doi:10.2807/esw.11.25.02977-en. PMID 16819127.
- ^ Lopes de Carvalho I, Núncio MS (2006). “Laboratory diagnosis of Lyme borreliosis at the Portuguese National Institute of Health (1990-2004)”. Euro Surveillance. 11 (10): 257–60. PMID 17130658. Archived from the original on 17 June 2012.
- ^ Jump up to:a b c d “Epidemiology of Lyme borreliosis in the UK”. HPA. Archived from the original on 10 June 2013. Retrieved 15 December 2012.
- ^ Muhlemann MF, Wright DJ (January 1987). “Emerging pattern of Lyme disease in the United Kingdom and Irish Republic”. Lancet. 1 (8527): 260–2. doi:10.1016/S0140-6736(87)90074-2. PMID 2880076. S2CID 25295954.
- ^ Jump up to:a b Lyme Disease Archived 15 June 2013 at the Wayback MachineHansard 11 November 1991
- ^ Jump up to:a b “Tick Lyme disease off your holiday list” (Press release). Health Protection Agency. 14 April 2011. Archived from the original on 28 April 2011. Retrieved 29 March 2013.
- ^ “Concern about rise in Lyme disease cases”. Lyme Disease Action. 15 December 2011. Archived from the original on 19 June 2013. Retrieved 15 December 2012.
- ^ Cassidy, Frank (14 March 2011). “Tayside revealed as a Lyme disease hotspot as cases soar”. Press and Journal. Archived from the original on 11 March 2016.
- ^ “Lyme disease: A clear and present danger”. RCN. 28 April 2009. Archived from the original on 29 March 2013. Retrieved 15 December 2012.
- ^ “Guidance on Part 2 – Notifiable Diseases, Notifiable Organisms and Health Risk States”. Scotland.gov.uk. 10 September 2012. Retrieved 15 December2012.
- ^ Lyme Disease Archived 15 June 2013 at the Wayback MachineHansard, 3 February 1997
- ^ Tick-Borne Disease, Risk and Realit Archived 20 November 2012 at the Wayback Machine BADA-UK, Wendy Fox, 2010
- ^ “Lyme borreliosis epidemiology and surveillance: May 2013”. HPA. Archived from the original on 25 November 2015. Retrieved 24 November2015.
- ^ “Zoonoses report UK 2009” (PDF). DEFRA. 24 January 2011. Archived(PDF) from the original on 3 November 2012.
- ^ Overview Tick Bite Prevention Week Archived 10 April 2012 at the Wayback Machine
- ^ Haywood GA, O’Connell S, Gray HH (July 1993). “Lyme carditis: a United Kingdom perspective”. British Heart Journal. 70 (1): 15–6. doi:10.1136/hrt.70.1.15. PMC 1025222. PMID 8037992.
- ^ Guy EC, Bateman DE, Martyn CN, Heckels JE, Lawton NF (March 1989). “Lyme disease: prevalence and clinical importance of Borrelia burgdorferi specific IgG in forestry workers”. Lancet. 1 (8636): 484–6. doi:10.1016/S0140-6736(89)91377-9. PMID 2563850. S2CID 39557628.
- ^ Smith FD, Ballantyne R, Morgan ER, Wall R (March 2012). “Estimating Lyme disease risk using pet dogs as sentinels”. Comparative Immunology, Microbiology and Infectious Diseases. 35 (2): 163–7. doi:10.1016/j.cimid.2011.12.009. PMID 22257866. Lay summary – Bristol University (25 January 2012).
- ^ Roberts, Michelle (24 January 2012). “Lyme disease risk from dogs ‘higher than thought‘“. BBC News. Archived from the original on 31 January 2012.
- ^ “The London climate change adaptation strategy – Draft report” (PDF). Greater London Authority. August 2008. Archived from the original (PDF) on 17 August 2012.
- ^ Brownstein JS, Holford TR, Fish D (March 2005). “Effect of Climate Change on Lyme Disease Risk in North America”. EcoHealth. 2 (1): 38–46. doi:10.1007/s10393-004-0139-x. PMC 2582486. PMID 19008966.
- ^ Jump up to:a b Killilea ME, Swei A, Lane RS, Briggs CJ, Ostfeld RS (June 2008). “Spatial dynamics of lyme disease: a review” (PDF). EcoHealth. 5 (2): 167–95. CiteSeerX 10.1.1.580.8928. doi:10.1007/s10393-008-0171-3. PMID 18787920. S2CID 13545850. Archived (PDF) from the original on 8 September 2015.
- ^ BC Ministry of Agriculture. “Ticks and Humans in British Columbia”. Agf.gov.bc.ca. Archived from the original on 3 January 2013. Retrieved 15 December 2012.
- ^ “Lyme Disease Fact Sheet”. Phac-aspc.gc.ca. 4 July 2012. Archivedfrom the original on 27 December 2012. Retrieved 15 December 2012.
- ^ Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H (June 2009). “The emergence of Lyme disease in Canada”. CMAJ. 180 (12): 1221–4. doi:10.1503/cmaj.080148. PMC 2691438. PMID 19506281.
- ^ Leighton PA, Koffi JK, Pelcat Y, Lindsay LR, Ogden NH (2012). “Predicting the speed of tick invasion: An empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada”. J. Appl. Ecol. 49 (2): 457–64. doi:10.1111/j.1365-2664.2012.02112.x. S2CID 16921155.
- ^ Gordillo-Pérez G, Torres J, Solórzano-Santos F, de Martino S, Lipsker D, Velázquez E, Ramon G, Onofre M, Jaulhac B (October 2007). “Borrelia burgdorferi infection and cutaneous Lyme disease, Mexico”. Emerging Infectious Diseases. 13 (10): 1556–8. doi:10.3201/eid1310.060630. PMC 2851501. PMID 18258006.
- ^ Jump up to:a b “Reported cases of Lyme disease by state or locality, 2005–2014†”. cdc.gov. 6 November 2017. Archived from the original on 4 May 2012.
- ^ “How many people get Lyme disease?”. cdc.gov. 21 December 2018. Archived from the original on 13 October 2014.
- ^ CDC (4 January 2012). “Reported Lyme disease cases by state, 2000-2010”. Centers for Disease Control and Prevention (CDC). Archived from the original on 4 May 2012. Retrieved 29 April 2012.
- ^ Centers for Disease Control Prevention (CDC) (June 2007). “Lyme disease—United States, 2003–2005”. MMWR. Morbidity and Mortality Weekly Report. 56 (23): 573–6. PMID 17568368. Archived from the original on 19 November 2012.
- ^ Bacon RM, Kugeler KJ, Mead PS (October 2008). “Surveillance for Lyme disease–United States, 1992-2006”. MMWR. Surveillance Summaries. 57(10): 1–9. PMID 18830214. Archived from the original on 10 November 2012.
- ^ Jump up to:a b Robbins, Jim (20 May 2003). “Montana Lab Tries to Identify Tick-Borne Disease”. The New York Times. Archived from the original on 3 September 2017.
- ^ “Lyme Disease Data” Archived 30 April 2012 at the Wayback Machine. Centers for Disease Control and Prevention (CDC).
- ^ “Lyme disease (Borrelia burgdorferi) 2011 case definition”. U.S. Centers for Disease Control and Prevention. Archived from the original on 22 April 2012.
- ^ Jump up to:a b “Lyme disease (Borrelia burgdorferi) 2008 case definition”. U.S. Centers for Disease Control and Prevention. Archived from the original on 12 June 2012.
- ^ Jump up to:a b Swanson KI, Norris DE (2007). “Detection of Borrelia burgdorferi DNA in lizards from Southern Maryland”. Vector Borne and Zoonotic Diseases. 7 (1): 42–9. doi:10.1089/vbz.2006.0548. PMC 4128253. PMID 17417956.
- ^ Richter D, Matuschka FR (July 2006). “Perpetuation of the Lyme disease spirochete Borrelia lusitaniae by lizards”. Applied and Environmental Microbiology. 72 (7): 4627–32. doi:10.1128/AEM.00285-06. PMC 1489336. PMID 16820453.
- ^ Giery ST, Ostfeld RS (June 2007). “The role of lizards in the ecology of Lyme disease in two endemic zones of the northeastern United States”. The Journal of Parasitology. 93 (3): 511–7. doi:10.1645/GE-1053R1.1. PMID 17626342. S2CID 42617030.
- ^ Amore G, Tomassone L, Grego E, Ragagli C, Bertolotti L, Nebbia P, Rosati S, Mannelli A (March 2007). “Borrelia lusitaniae in immature Ixodes ricinus (Acari: Ixodidae) feeding on common wall lizards in Tuscany, central Italy”. Journal of Medical Entomology. 44 (2): 303–7. doi:10.1603/0022-2585(2007)44[303:BLIIIR]2.0.CO;2. PMID 17427701.
- ^ Majláthová V, Majláth I, Derdáková M, Víchová B, Pet’ko B (December 2006). “Borrelia lusitaniae and green lizards (Lacerta viridis), Karst Region, Slovakia”. Emerging Infectious Diseases. 12 (12): 1895–901. doi:10.3201/eid1212.060784. PMC 3291370. PMID 17326941.
- ^ “STARI or Lyme?”. Centers for Disease Control and Prevention. 19 November 2018. Archived from the original on 12 November 2019.
- ^ Lyme disease fact sheet Analysis of CDC data on VoxHealth. Retrieved on 2013-30-1
- ^ Mantovani E, Costa IP, Gauditano G, Bonoldi VL, Higuchi ML, Yoshinari NH (April 2007). “Description of Lyme disease-like syndrome in Brazil. Is it a new tick borne disease or Lyme disease variation?”. Brazilian Journal of Medical and Biological Research = Revista Brasileira de Pesquisas Medicas e Biologicas. 40 (4): 443–56. doi:10.1590/S0100-879X2006005000082. PMID 17401487.
- ^ Yoshinari NH, Oyafuso LK, Monteiro FG, de Barros PJ, da Cruz FC, Ferreira LG, Bonasser F, Baggio D, Cossermelli W, et al. (1993). “[Lyme disease. Report of a case observed in Brazil]” [Lyme disease. Report of a case observed in Brazil]. Revista do Hospital das Clinicas (in Portuguese). 48 (4): 170–4. PMID 8284588.
- ^ Palacios, Ricardo; Torres, Antonio; Trujillo, Rodolfo (November 2003). “IgG antibody reactivity to Borrelia burgdorferi sensu stricto antigens in patients with morphea in Colombia”. International Journal of Dermatology. 42 (11): 882–6. doi:10.1046/j.1365-4362.2003.01901.x. PMID 14636204. S2CID 24927804.
- ^ Hoen AG, Margos G, Bent SJ, Diuk-Wasser MA, Barbour A, Kurtenbach K, Fish D (September 2009). “Phylogeography of Borrelia burgdorferi in the eastern United States reflects multiple independent Lyme disease emergence events”. Proceedings of the National Academy of Sciences of the United States of America. 106 (35): 15013–8. Bibcode:2009PNAS..10615013H. doi:10.1073/pnas.0903810106. JSTOR 40484546. PMC 2727481. PMID 19706476. Lay summary – YaleNews (10 August 2009).
- ^ Josselyn, John (1670). An Account of Two Voyages to New-England Made during the Years 1638, 1663. Archived from the original on 25 June 2013.page 92
- ^ Jump up to:a b Drymon, MM (2008). Disguised as the devil: how Lyme disease created witches and changed history. pp. 51–52. ISBN 978-0-615-20061-3.
- ^ Summerton N (1995). “Lyme disease in the eighteenth century”. BMJ. 311(7018): 1478. doi:10.1136/bmj.311.7018.1478. S2CID 70661702.
- ^ Hall, Stephen S (November 2011). “Iceman Autopsy”. National Geographic. Archived from the original on 19 October 2011. Retrieved 17 October 2011.
- ^ Jump up to:a b Marcus, Karl (1910). “Verhandlungen der dermatologischen Gesellschaft zu Stockholm”. Arch. Dermatol. Syph. 101 (2–3): 403–06. doi:10.1007/BF01832773. S2CID 46704791.
- ^ Burckhardt JL (1911). “Zur Frage der Follikel- und Keimzentrenbildung in der Haut”. Frankf. Z. Pathol. (in German). 6: 352–59.
- ^ Edlow, Jonathan A (2003). Bull’s-eye: unraveling the medical mystery of Lyme disease. Yale University Press. ISBN 978-0-300-09867-9. page 191.
- ^ Hellerström S (1930). “Erythema chronicum migrans Afzelii“. Acta Derm.-Venerol. (in German). 11: 315–21.
- ^ Lenhoff C (1948). “Spirochetes in aetiologically obscure diseases”. Acta Derm.-Venerol. 28 (3): 295–324. PMID 18891989.
- ^ Thyresson N (1949). “The penicillin treatment of acrodermatitis atrophicans chronica (Herxheimer)”. Acta Dermato-Venereologica. 29 (6): 572–621. PMID 18140373.
- ^ Bianchi GE (1950). “[Penicillin therapy of lymphocytoma]” [Penicillin therapy of lymphocytoma]. Dermatologica (in German). 100 (4–6): 270–3. doi:10.1159/000257185. PMID 15421023.
- ^ Paschoud JM (1954). “[Lymphocytoma after tick bite]” [Lymphocytoma after tick bite]. Dermatologica (in German). 108 (4–6): 435–7. PMID 13190934.
- ^ Scrimenti RJ (July 1970). “Erythema chronicum migrans”. Archives of Dermatology. 102 (1): 104–5. doi:10.1001/archderm.102.1.104. PMID 5497158.
- ^ Borchers AT, Keen CL, Huntley AC, Gershwin ME (February 2015). “Lyme disease: a rigorous review of diagnostic criteria and treatment”. Journal of Autoimmunity. 57: 82–115. doi:10.1016/j.jaut.2014.09.004. PMID 25451629.
- ^ Weir, William (19 September 2013). “Lyme Disease Pioneer Stephen Malawista Dies”. Hartford Courant. Archived from the original on 14 October 2013. Retrieved 14 October 2013.
- ^ Sternbach G, Dibble CL (1996). “Willy Burgdorfer: Lyme disease”. The Journal of Emergency Medicine. 14 (5): 631–4. doi:10.1016/S0736-4679(96)00143-6. PMID 8933327.
- ^ Bolognia JL, Jorizzo JL, Rapini RP (2007). Dermatology (2nd ed.). St. Louis: Mosby. ISBN 978-1-4160-2999-1.[page needed]
- ^ Mast WE, Burrows WM (November 1976). “Erythema chronicum migrans and “lyme arthritis““. JAMA. 236 (21): 2392d–2392. doi:10.1001/jama.236.21.2392d. PMID 989847.
- ^ Steere AC, Malawista SE, Snydman DR, Shope RE, Andiman WA, Ross MR, Steele FM (1977). “Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three connecticut communities”. Arthritis and Rheumatism. 20 (1): 7–17. doi:10.1002/art.1780200102. PMID 836338.
- ^ “Factsheet about Borreliosis”. European Centre for Disease Prevention and Control. Archived from the original on 27 September 2019. Retrieved 30 January 2020.
- ^ “WHO | Lyme Borreliosis (Lyme disease)”. WHO. Archived from the original on 29 November 2019. Retrieved 30 January 2020.
- ^ Steere AC, Hutchinson GJ, Rahn DW, Sigal LH, Craft JE, DeSanna ET, Malawista SE (July 1983). “Treatment of the early manifestations of Lyme disease”. Annals of Internal Medicine. 99 (1): 22–6. doi:10.7326/0003-4819-99-1-22. PMID 6407378.
- ^ Burgdorfer W (1984). “Discovery of the Lyme disease spirochete and its relation to tick vectors”. The Yale Journal of Biology and Medicine. 57 (4): 515–20. PMC 2590008. PMID 6516454.
- ^ Burgdorfer W, Barbour AG, Hayes SF, Benach JL, Grunwaldt E, Davis JP (June 1982). “Lyme disease-a tick-borne spirochetosis?”. Science(Submitted manuscript). 216 (4552): 1317–9. Bibcode:1982Sci…216.1317B. doi:10.1126/science.7043737. PMID 7043737. Archived from the original on 30 January 2020. Retrieved 4 September 2018.
- ^ Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ (1988). “New chemotherapeutic approaches in the treatment of Lyme borreliosis”. Annals of the New York Academy of Sciences. 539 (1): 352–61. Bibcode:1988NYASA.539..352L. doi:10.1111/j.1749-6632.1988.tb31869.x. PMID 3056203. S2CID 25939418.
- ^ Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ (December 1990). “Amoxycillin plus probenecid versus doxycycline for treatment of erythema migrans borreliosis”. Lancet. 336 (8728): 1404–6. doi:10.1016/0140-6736(90)93103-V. PMID 1978873. S2CID 7314488.
- ^ Ribeiro JM, Mather TN, Piesman J, Spielman A (March 1987). “Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae)”. Journal of Medical Entomology. 24 (2): 201–5. doi:10.1093/jmedent/24.2.201. PMID 3585913.
- ^ LoGiudice K, Ostfeld RS, Schmidt KA, Keesing F (January 2003). “The ecology of infectious disease: effects of host diversity and community composition on Lyme disease risk”. Proceedings of the National Academy of Sciences of the United States of America. 100 (2): 567–71. Bibcode:2003PNAS..100..567L. doi:10.1073/pnas.0233733100. PMC 141036. PMID 12525705.
- ^ Patz JA, Daszak P, Tabor GM, Aguirre AA, Pearl M, Epstein J, Wolfe ND, Kilpatrick AM, Foufopoulos J, Molyneux D, Bradley DJ (July 2004). “Unhealthy landscapes: Policy recommendations on land use change and infectious disease emergence”. Environmental Health Perspectives. 112 (10): 1092–8. doi:10.1289/ehp.6877. PMC 1247383. PMID 15238283.
- ^ Khasnis AA, Nettleman MD (2005). “Global warming and infectious disease”. Archives of Medical Research. 36 (6): 689–96. doi:10.1016/j.arcmed.2005.03.041. PMID 16216650.
- ^ Feder HM, Johnson BJ, O’Connell S, Shapiro ED, Steere AC, Wormser GP, Agger WA, Artsob H, Auwaerter P, Dumler JS, Bakken JS, Bockenstedt LK, Green J, Dattwyler RJ, Munoz J, Nadelman RB, Schwartz I, Draper T, McSweegan E, Halperin JJ, Klempner MS, Krause PJ, Mead P, Morshed M, Porwancher R, Radolf JD, Smith RP, Sood S, Weinstein A, Wong SJ, Zemel L (October 2007). “A critical appraisal of “chronic Lyme disease““. The New England Journal of Medicine. 357 (14): 1422–30. doi:10.1056/NEJMra072023. PMID 17914043. S2CID 35285261.
- ^ ““Chronic Lyme Disease” Fact Sheet”. National Institute of Allergy and Infectious Diseases. 17 April 2009. Archived from the original on 15 December 2012.
- ^ Marques A (June 2008). “Chronic Lyme disease: a review”. Infectious Disease Clinics of North America. 22 (2): 341–60, vii–viii. doi:10.1016/j.idc.2007.12.011. PMC 2430045. PMID 18452806.
- ^ Holden, Stephen (19 June 2009). “Ticked Off”. New York Times. Retrieved 6 January 2009.
- ^ “How a Rock Musician Inspired One Family Dealing With Lyme Disease”. HuffPost. 7 July 2014. Retrieved 30 January 2021.
- ^ “Kyle Morton: The Unlikely Saxon”. PDX Magazine. Retrieved 30 January2021.
- ^ Jump up to:a b Little SE, Heise SR, Blagburn BL, Callister SM, Mead PS (April 2010). “Lyme borreliosis in dogs and humans in the USA”. Trends in Parasitology. 26(4): 213–8. doi:10.1016/j.pt.2010.01.006. PMID 20207198.
- ^ Jump up to:a b Krupka I, Straubinger RK (November 2010). “Lyme borreliosis in dogs and cats: background, diagnosis, treatment and prevention of infections with Borrelia burgdorferi sensu stricto”. The Veterinary Clinics of North America. Small Animal Practice. 40 (6): 1103–19. doi:10.1016/j.cvsm.2010.07.011. PMID 20933139.
- ^ Hahn, Jeffrey. “Ticks and Their Control”. Regents of the University of Minnesota. Archived from the original on 25 February 2012. Retrieved 19 February 2012.
- ^ “Glomerular Disease”. The Merck Veterinary Manual. Archived from the original on 26 June 2017. Retrieved 19 May 2017.
- ^ Staubinger, PhD, R. (31 May 2000). “Lyme Disease”. Sirius Dog. Archived from the original on 23 June 2012. Retrieved 10 February2012.[unreliable source?]
- ^ Fatal cases of Lyme disease reported in the medical literature include:
- Kirsch M, Ruben FL, Steere AC, Duray PH, Norden CW, Winkelstein A (May 1988). “Fatal adult respiratory distress syndrome in a patient with Lyme disease”. JAMA. 259 (18): 2737–9. doi:10.1001/jama.1988.03720180063034. PMID 3357244.
- Oksi J, Kalimo H, Marttila RJ, Marjamäki M, Sonninen P, Nikoskelainen J, Viljanen MK (December 1996). “Inflammatory brain changes in Lyme borreliosis. A report on three patients and review of literature”. Brain. 119 ( Pt 6) (Pt 6): 2143–54. doi:10.1093/brain/119.6.2143. PMID 9010017.
- Waniek C, Prohovnik I, Kaufman MA, Dwork AJ (1995). “Rapidly progressive frontal-type dementia associated with Lyme disease”. The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (3): 345–7. doi:10.1176/jnp.7.3.345. PMID 7580195.
- Cary NR, Fox B, Wright DJ, Cutler SJ, Shapiro LM, Grace AA (February 1990). “Fatal Lyme carditis and endodermal heterotopia of the atrioventricular node”. Postgraduate Medical Journal. 66 (772): 134–6. doi:10.1136/pgmj.66.772.134. PMC 2429516. PMID 2349186.
- ^ Spears, Tom (4 January 2019). “Blood-sucking ticks are killing young moose at an alarming rate | Ottawa Citizen”. Archived from the original on 15 December 2019. Retrieved 15 December 2019.
- ^ “Chronic Lyme Disease”. National Institute of Allergy and Infectious Diseases. Archived from the original on 15 December 2012. Retrieved 15 October 2013.
![]() This article incorporates public domain material from the Centers for Disease Control and Prevention document: “Post-Treatment Lyme Disease Syndrome”.
This article incorporates public domain material from the Centers for Disease Control and Prevention document: “Post-Treatment Lyme Disease Syndrome”.
Further reading[edit]
- Richard Ostfeld (2012). Lyme Disease: The Ecology of a Complex System. New York: Oxford University Press. ISBN 978-0199928477.
- Pamela Weintraub (2008). Cure Unknown: Inside the Lyme Disease Epidemic. St. Martin’s Press. ISBN 9780312378127.
- Newby, Kris (2019). Bitten: the Secret History of Lyme Disease and Biological Weapons. HarperCollins. ISBN 9780062896278.
External links[edit]
| Wikimedia Commons has media related to Borreliosis. |
Lyme disease Flått Skaumann
Ixcodes ricinus Borrelia
Flåttmidden (Den klassiske: Ixodes ricinus, 8 ben) er trolig det farligste dyr for mennesker i Norden! Livssyklus: egg, larve, nymfe og voksen. Nymfene smittes fra mus. Noen mikrober: 1. Borreliose. Minst fem arter av Borreliaarten. Hyppigst Borrelia burgdorferi. Ofte rødt utslett/ ring rundt bittet. Mikrobene kan gå i dvale! Ny art: Borrelia miyamotoi. “Ikke utslett”. 2. TBE (Tick-borne encephalitis). Hjernebetennelse. Vaksine! 3. Rickettsia helvetica. Bakterien kan gi hjerterytmeforstyrrelse. 4. Neoehrlichia mikurensis. Bakterien kan gi influensaliknende symptomer og blodpropp (ofte). 5. Bartonella henselae. Bakterien fra flått til katt til menneske. Hjerteklaffbetennelse, hjernehinnebetennelse. 6. Babesia. Parasitt- likner på malaria. Ødelegger blodlegemer. Ofte hos hunder og kveg. I mikroskop: Maltese crosses in erythrocytes.
I helsevesenet er der stor uenighet om hvordan man skal behandle pasientene som er angrepet av borrelia. Det offentlige helsevesen er restriktiv med å utøve lengere penicillinbehandlig, mulig dette uten skikkelig vitenskaplig vurdering!
Hvordan man påviser borrelia er også uklart/ usikkert. Det finnes for dårlige påvisningsmetoder!
Trolig vet man ennå for lite om påvisning av borrelia og også om behandlingsopplegg.
Borreliabakterien går ofte over i cysteform (“spheroplast”), som trolig kan være vanskelig å angripe med medikamenter.
Tenk på: Det tok f.eks. lang tid før man kunne påvise TBC-bakterien, Denne bakterien har langsom intermiterende metabolisme, og her mot denne bakterien bruker man langtidskombinasjon av medikamenter. Selv om man mener at borrelia er sensitiv for kortidsbehandling med penicillin, kan mulig langtidsbehandling/ kombinasjon av medikamenter være riktig i en del tilfeller, når bakteriene er såpass spesielle (se også trippelbehandling ved helikobakterpåvisning i magesekk- mot mavesår. Les historien!).
Leger må ikke være så skåsikre!! Historien har flere ganger vist at det var feiloppfattning på et tidligere tidspunkt!
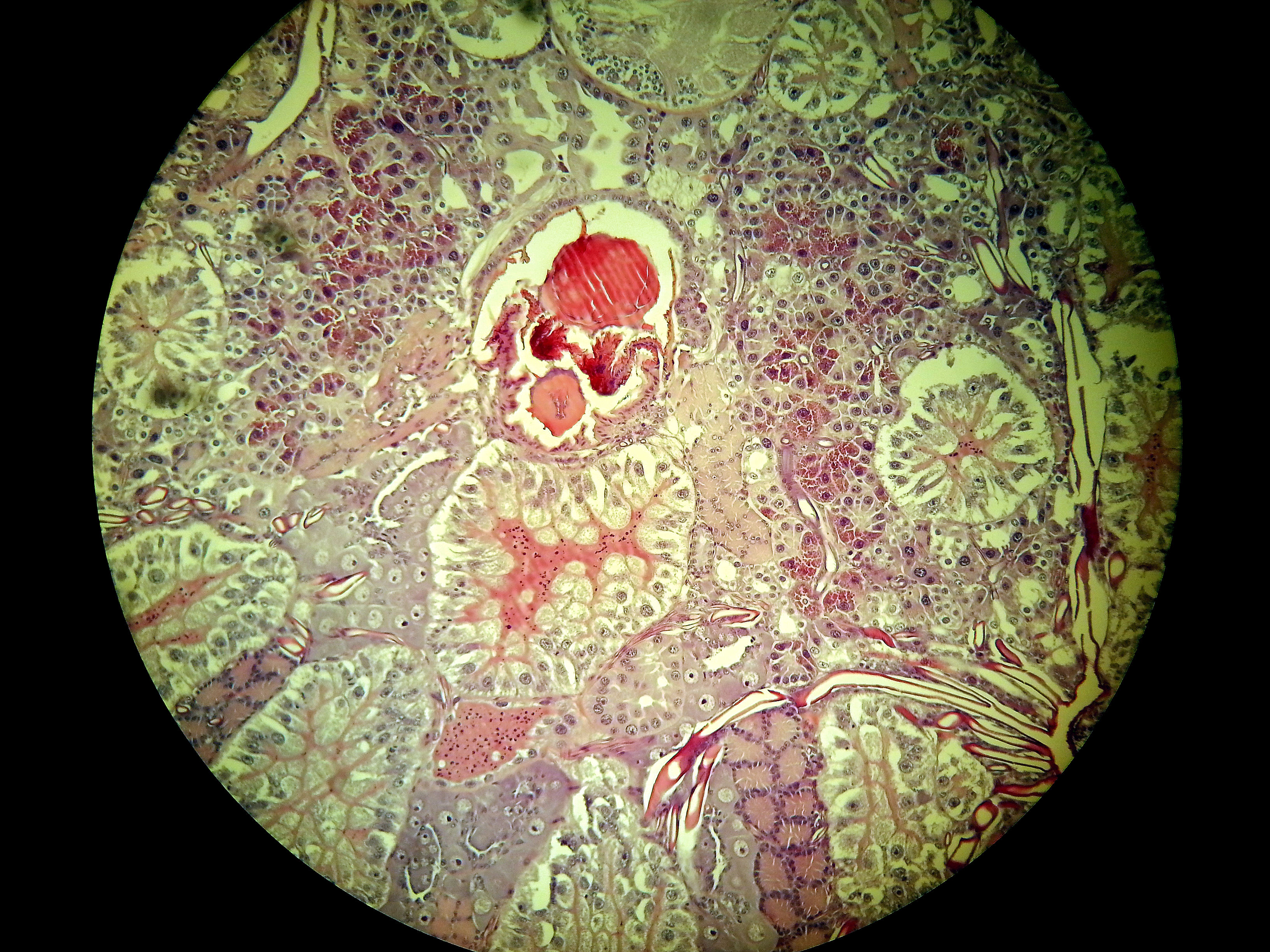 |
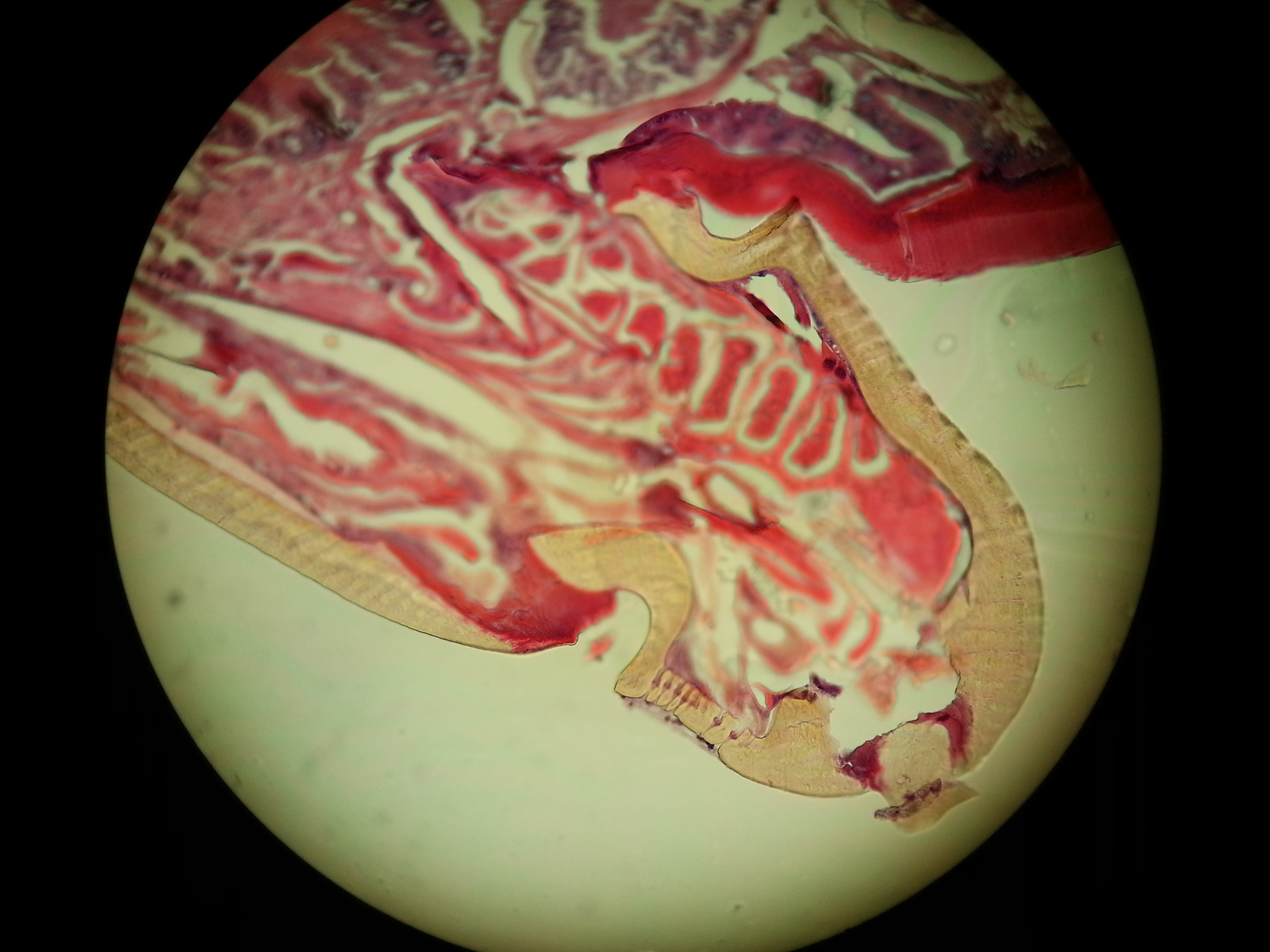
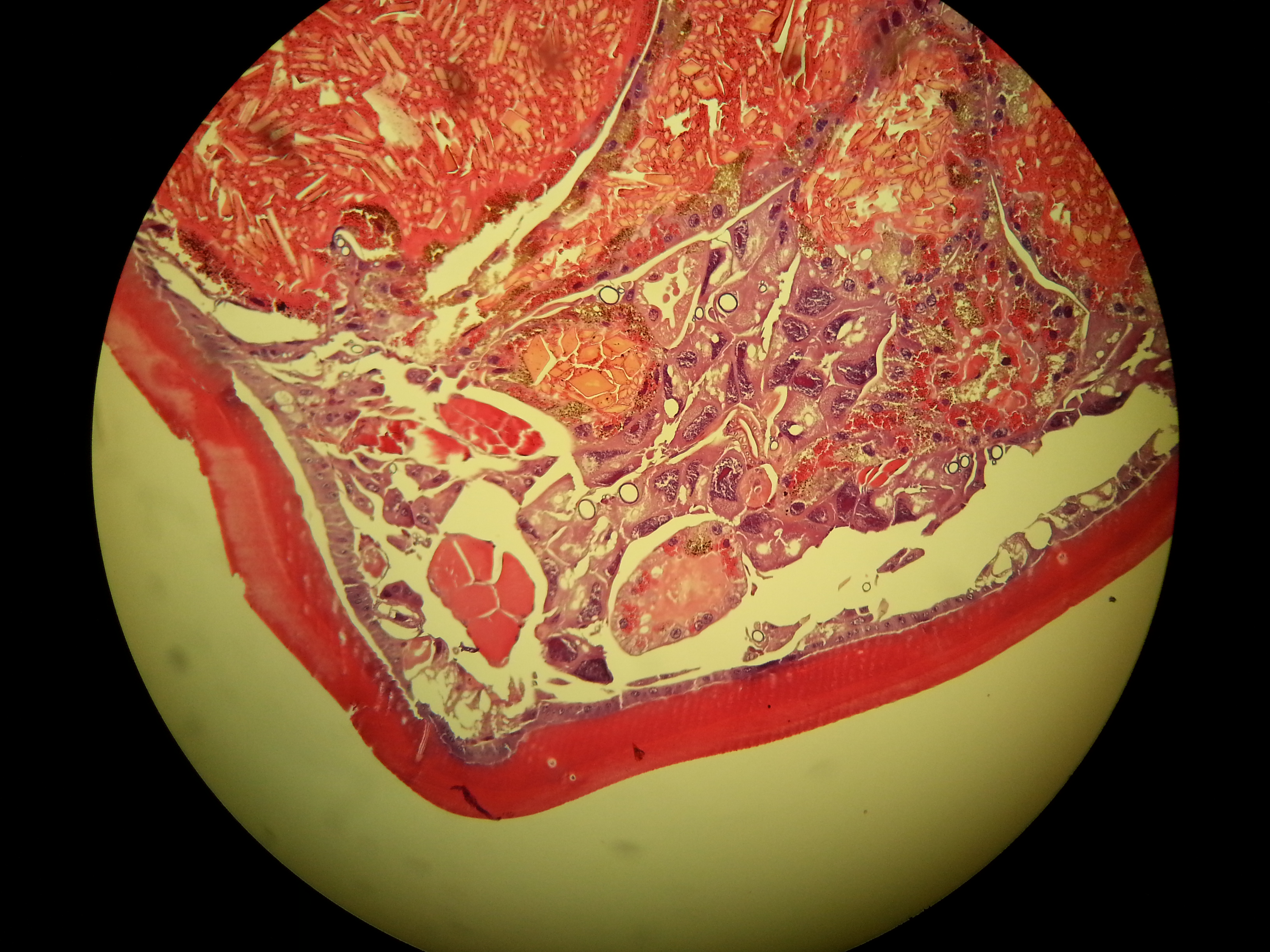
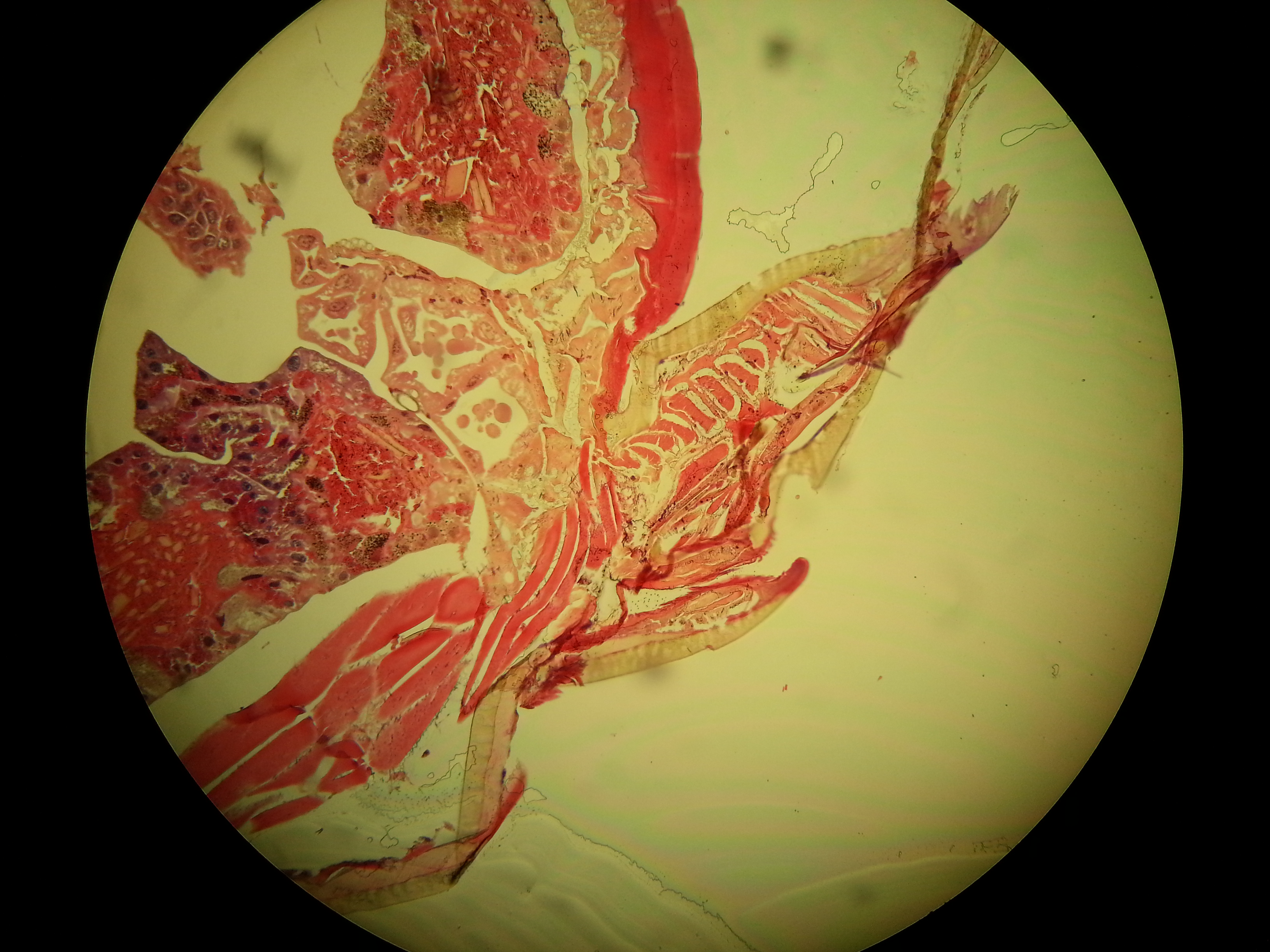
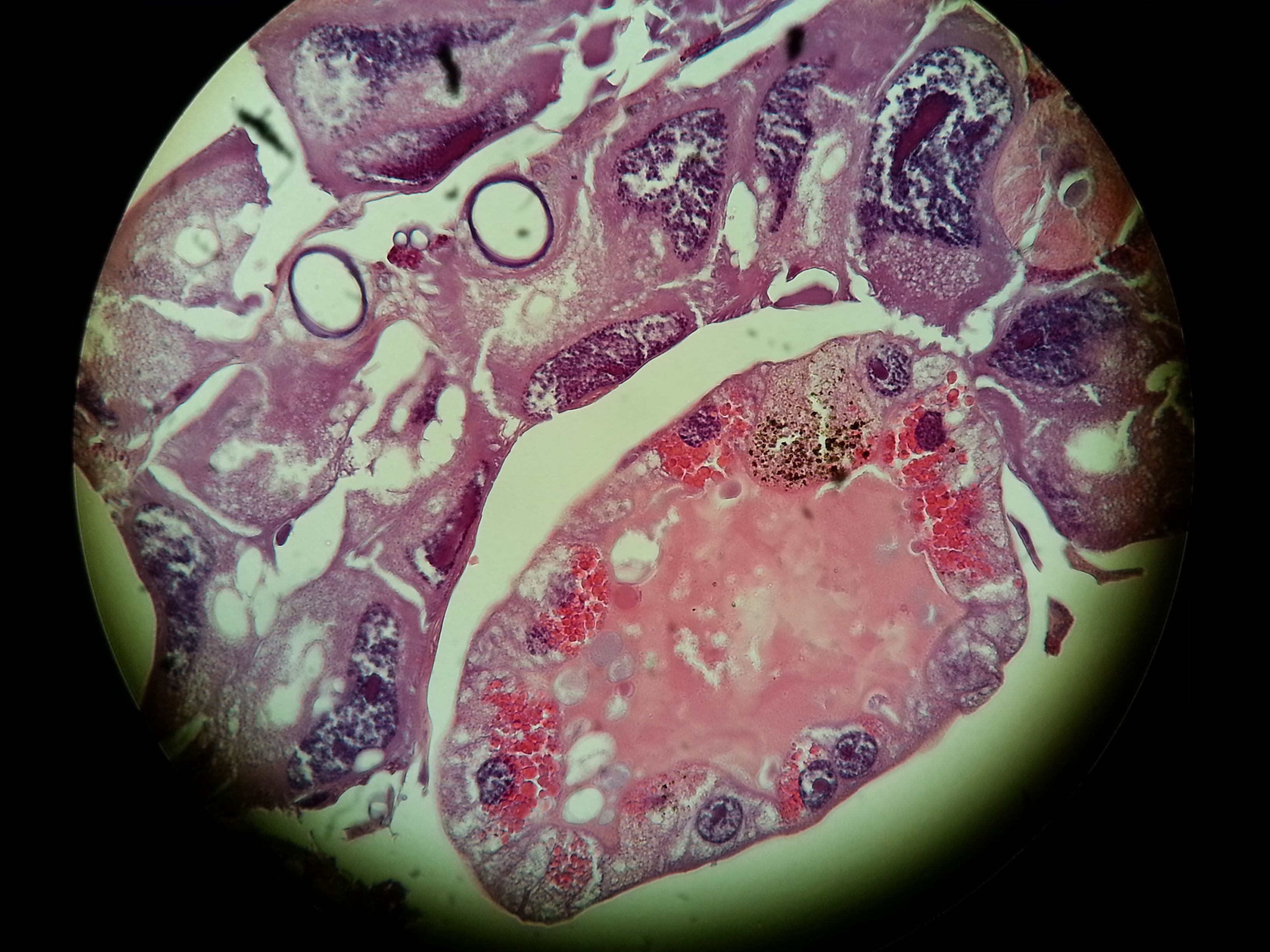
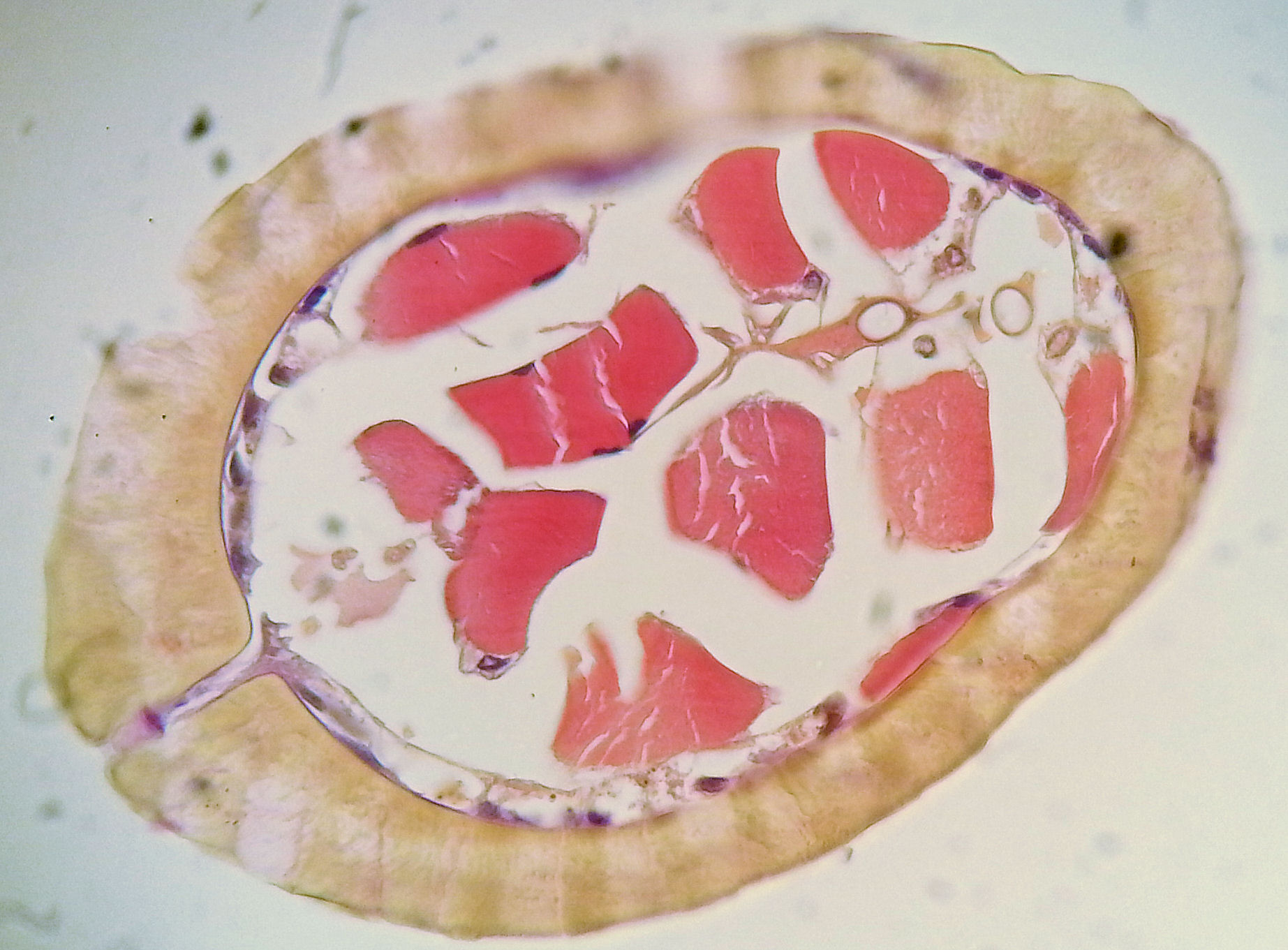



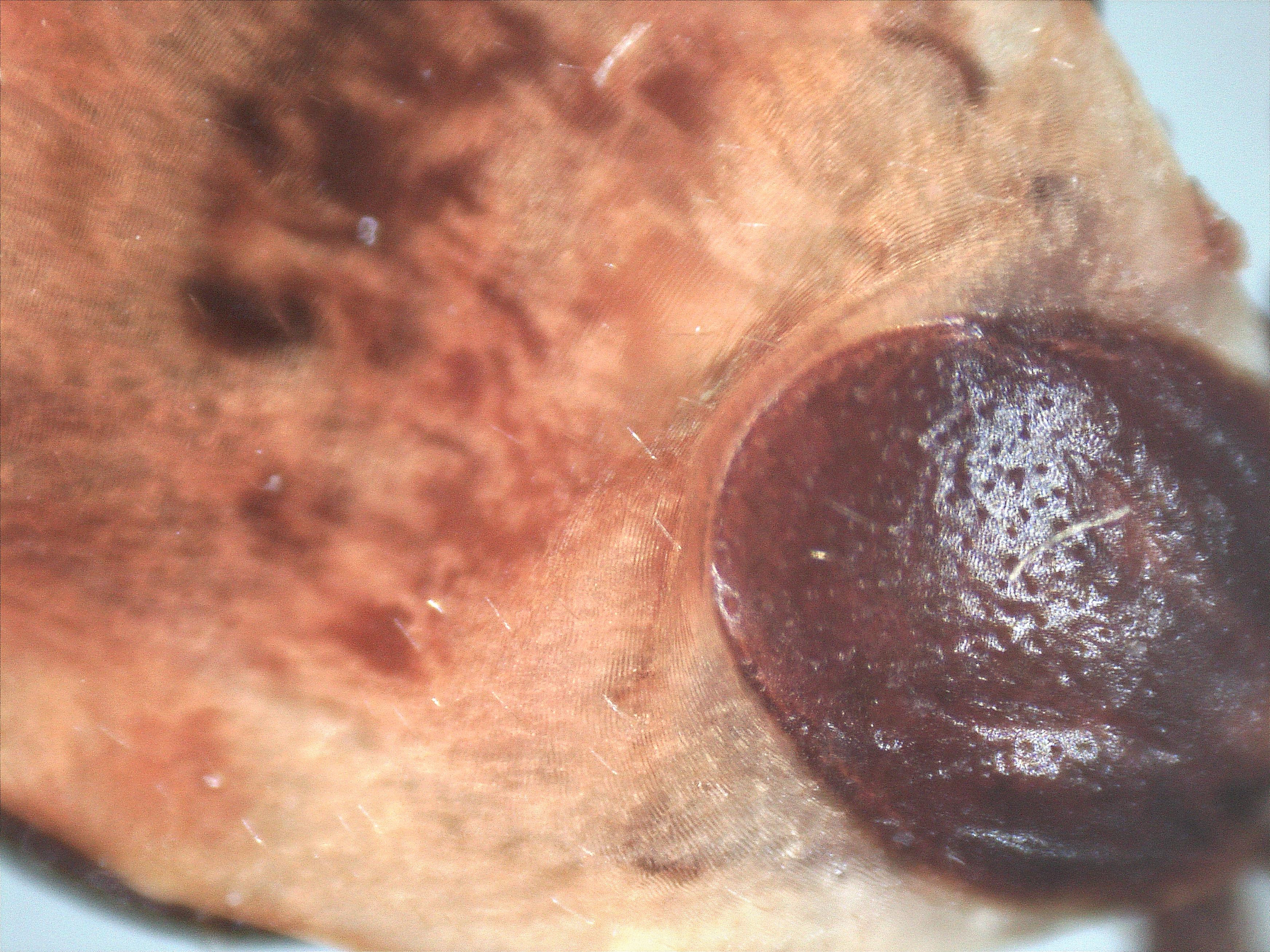

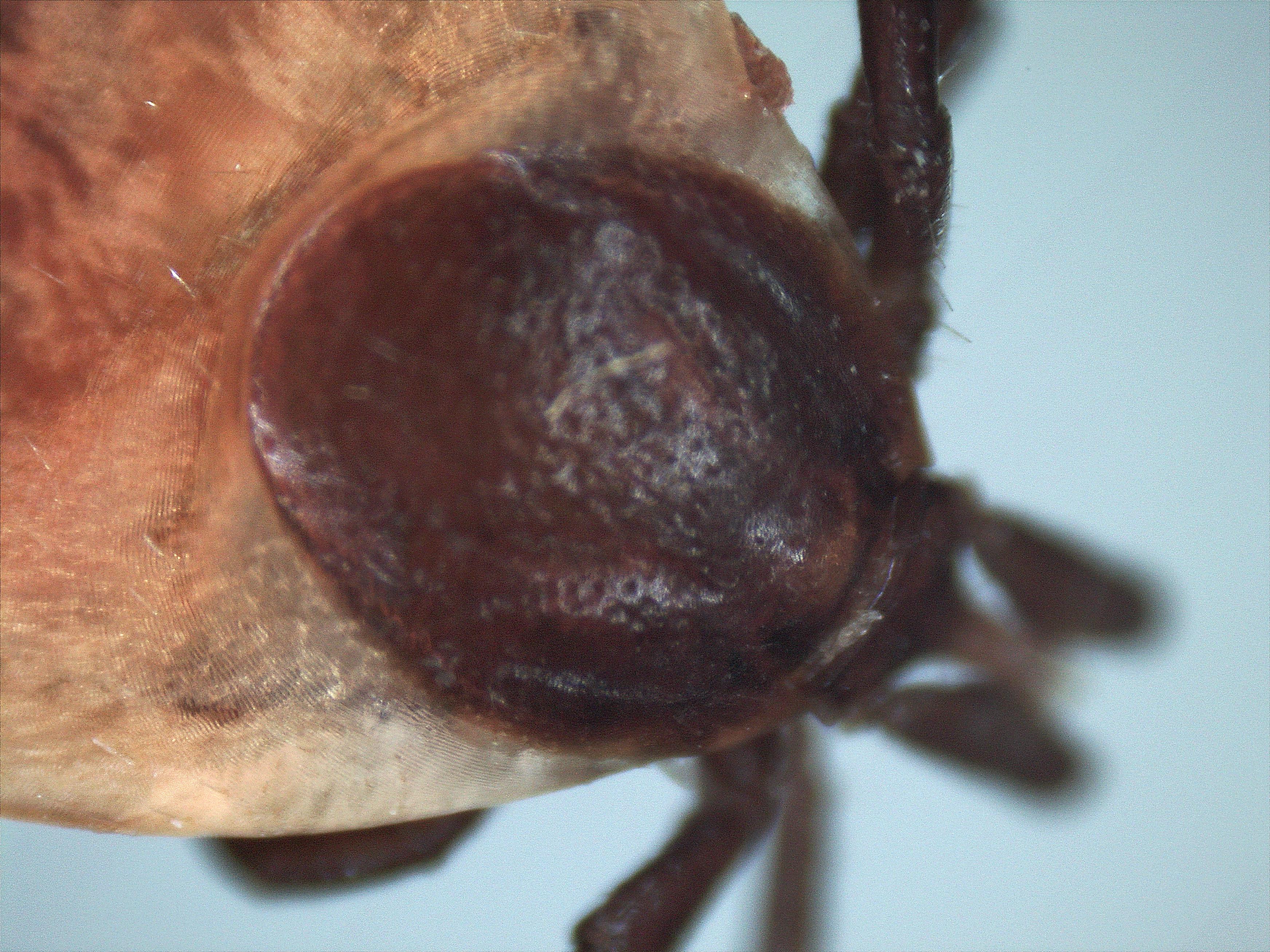

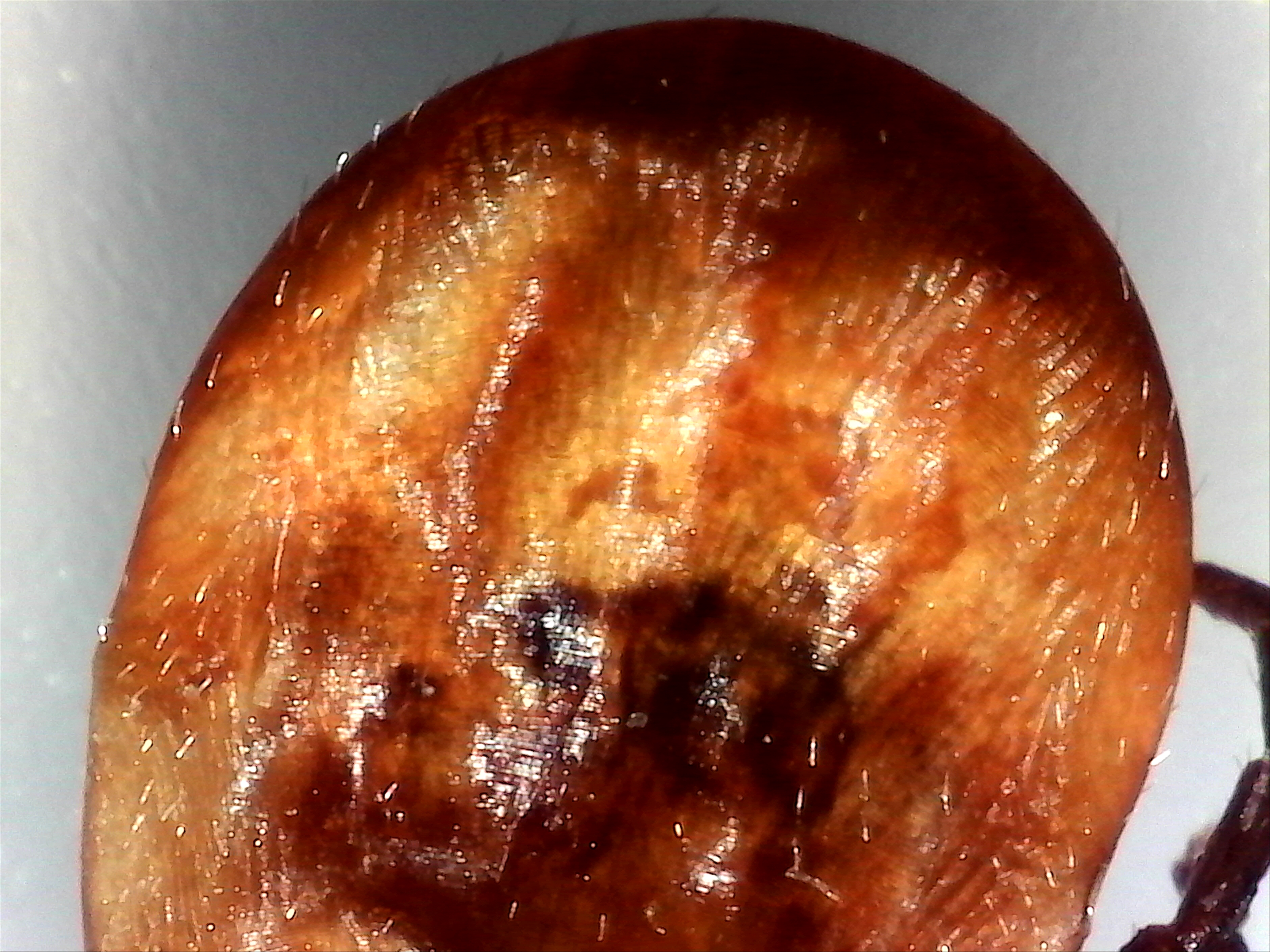
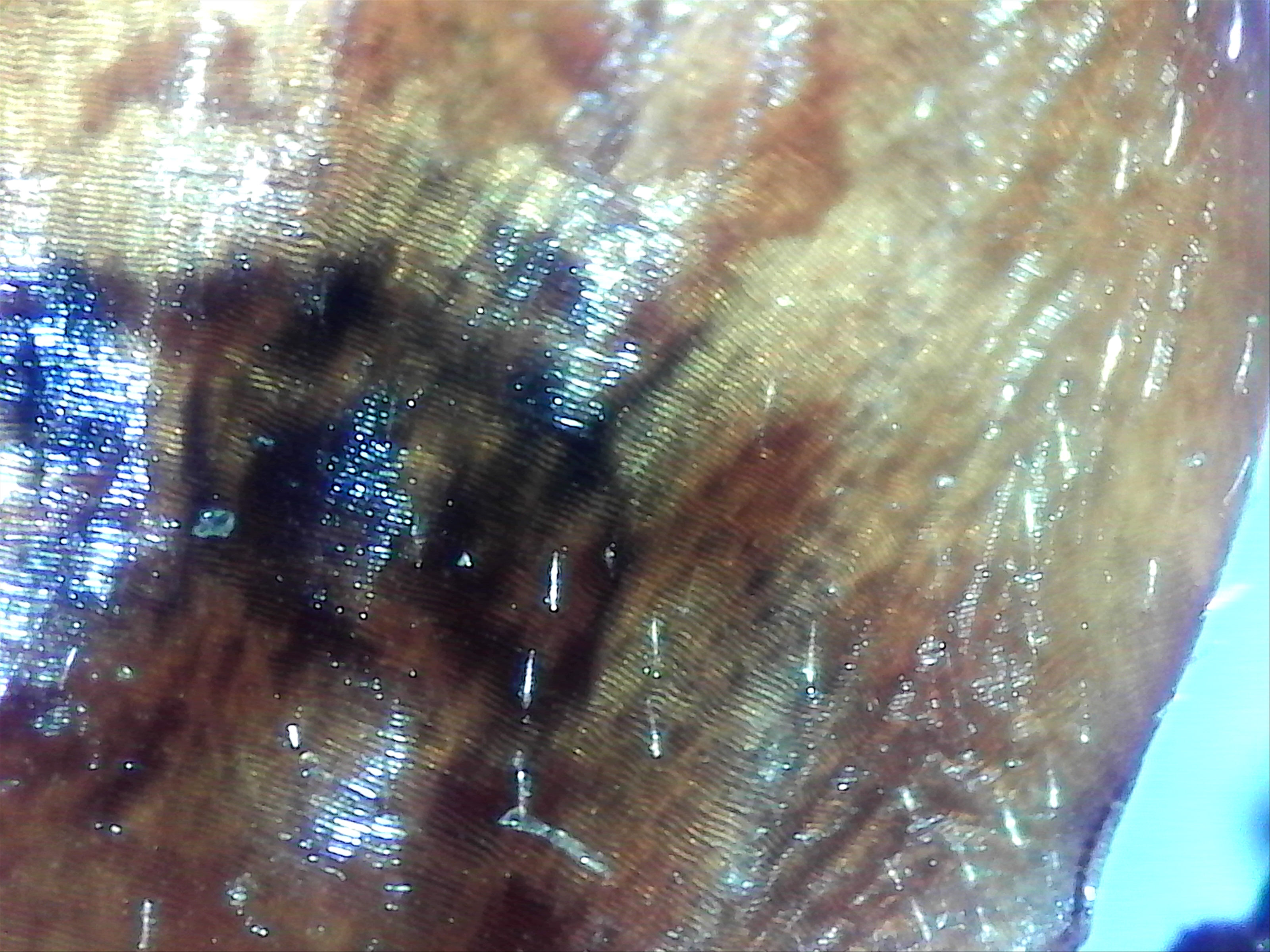
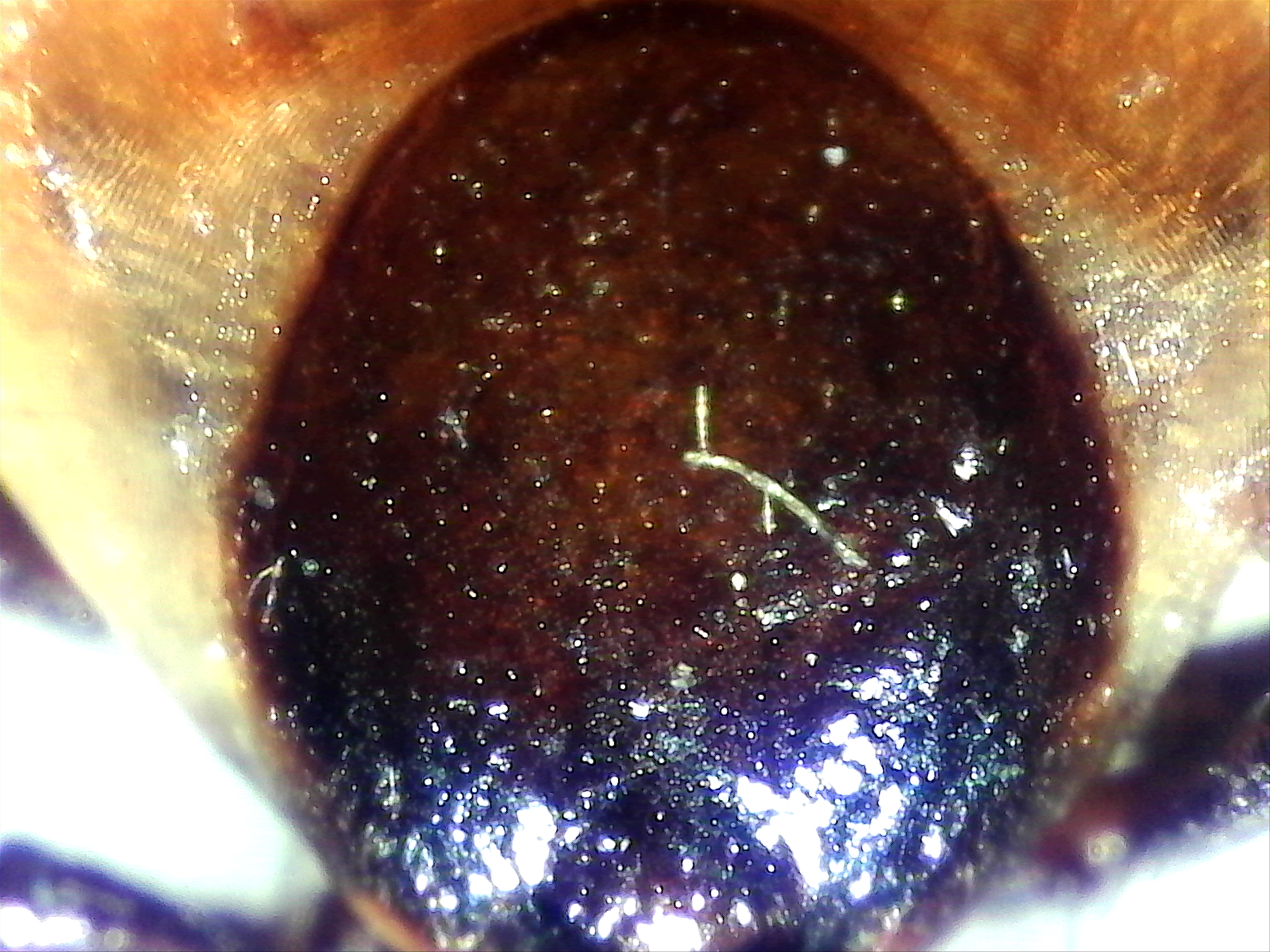
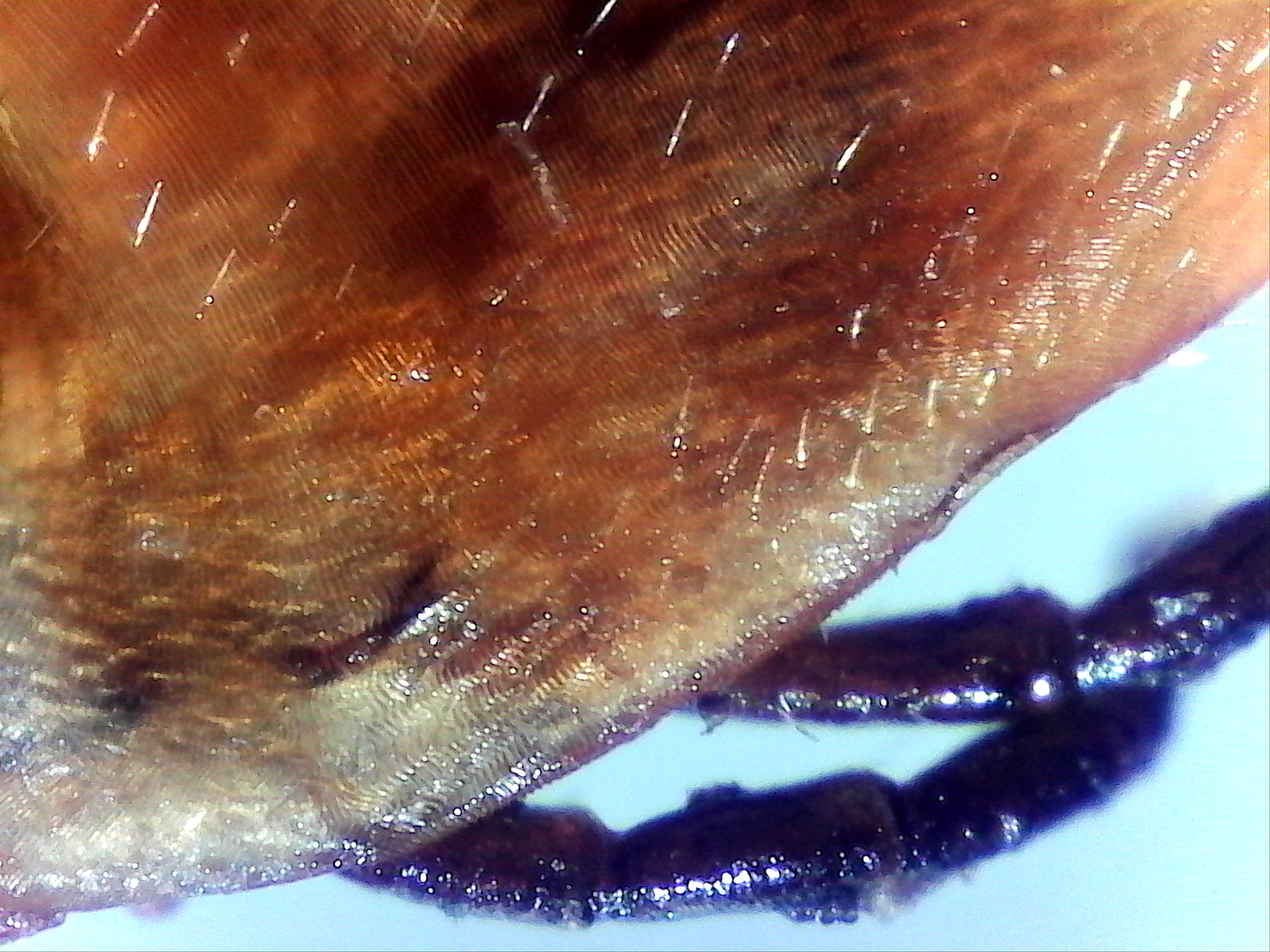

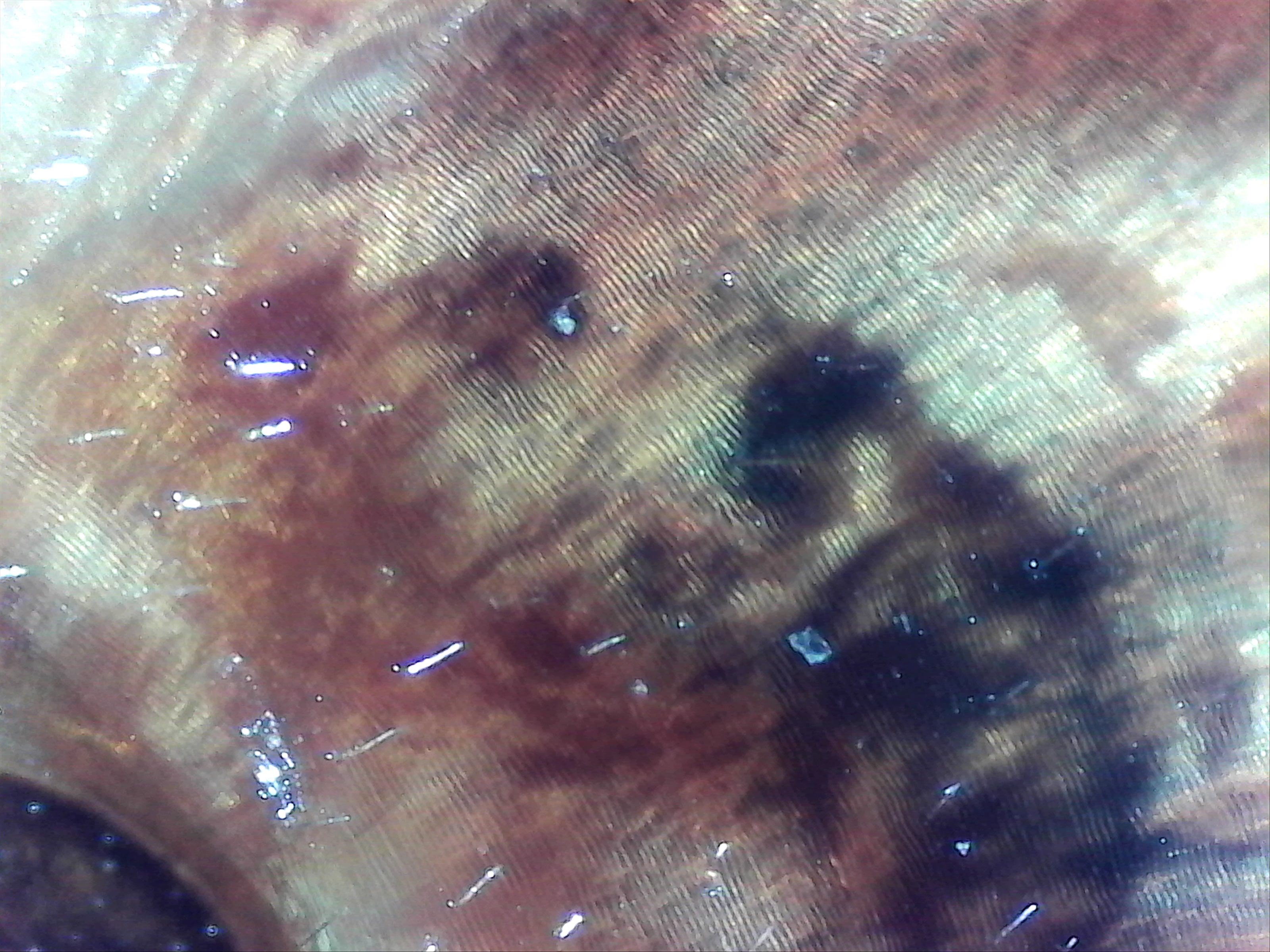




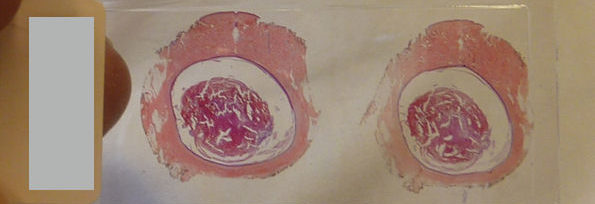






 Views Today : 1952
Views Today : 1952